From a practical clinical point of view, after the 2016 update of the SSC (Surviving Sepsis Campaign) guidelines we have two references when comes to deal with a potential septic patient. 
2016 Sepsis 3 definition and early management.
2016 Surviving Sepsis Campaign
Let’s see how to treat, based on top evidences, a real patient in the the pre-hospital and emergency department time window.
But, first of all, the definitions:
-
Definitions
Both the guidelines now agree that:
“Sepsis should be defined as life-threatening organ dysfunction caused by a dysregulated host response to infection“
“Septic shock should be defined as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by a vasopressor requirement to maintain a mean arterial pressure of 65 mm Hg or greater and serum lactate level greater than 2 mmol/L (>18 mg/dL) despite adequate volume resuscitation”
-
Early identification
- SIRS criteria. The new 2016 SSC guidelines do not indicate any criteria for early identification of sepsis, so SIRS criteria no longer exists.
- qSOFA score (G.C.S. of 13 or less, SBP of 100 mm Hg or less, and RR 22/min or greater): Good negative and positive prediction value(similar to that
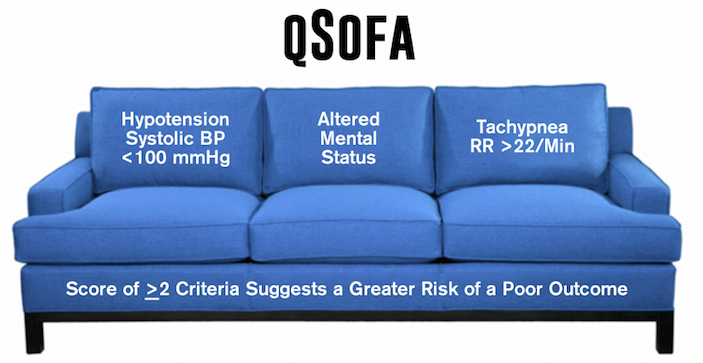 of the full SOFA score outside the ICU). Non specific for sepsis. It’s the actual early identification tool for sepsis to use out-of-hospital end in emergency department. It performs quite good to identify patients at risk of negative evolution. A qSOFA score ≥2 indicates a high mortality risk comparing to a qSOFA ≤1.
of the full SOFA score outside the ICU). Non specific for sepsis. It’s the actual early identification tool for sepsis to use out-of-hospital end in emergency department. It performs quite good to identify patients at risk of negative evolution. A qSOFA score ≥2 indicates a high mortality risk comparing to a qSOFA ≤1.
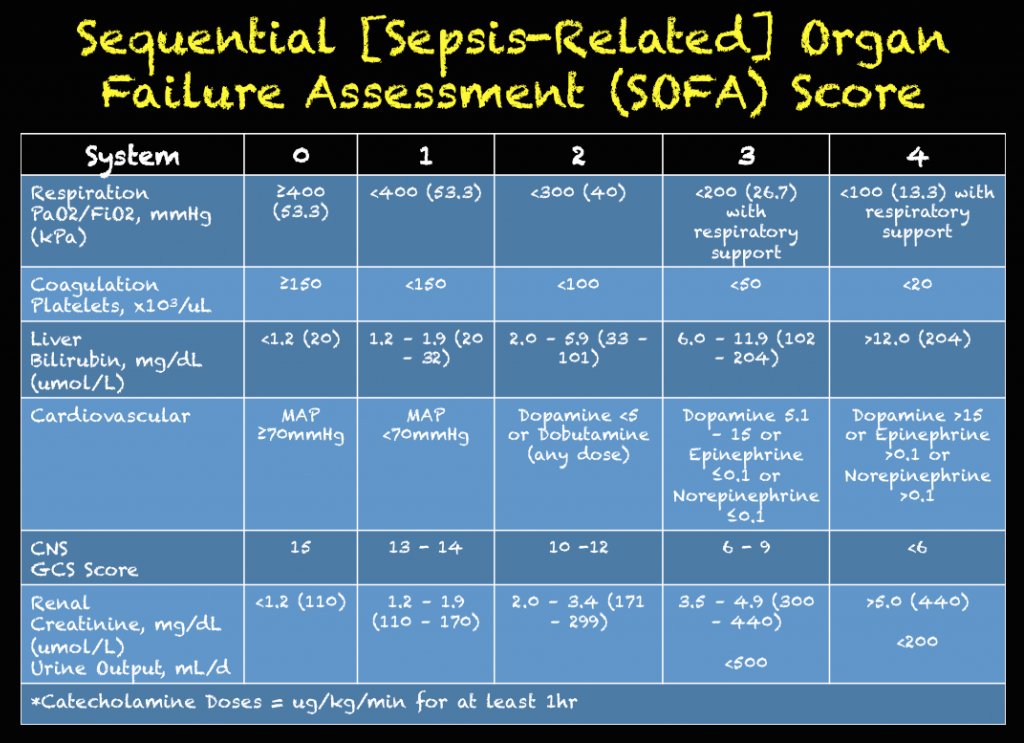
- SOFA score: indicates organ disfunction (when the score is >2 points) consequent to the infection and defines sepsis. Is a validated ICU tool to asses risk and mortality chance. Is not a tool to use out-of-hospital or in ED.
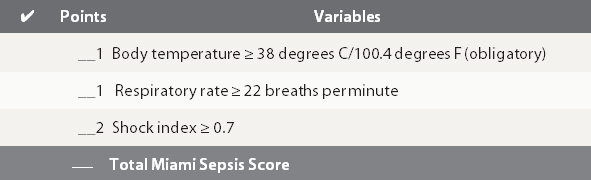
- The Pre-hospital Sepsis Score (PSS) or Miami Sepsis Score: As out-of-hospital professional I love pre-hospital early warning tools.I like to mention PSS cause is well validated to early recognise sepsis in the field. PSS includes Shock Index (HR/SBP) that is really sensible to identify critical evolution chance, RR that is included in qSOFA and other sepsis score plus body temperature (obligatory) that identifies an infection. Is for me the good compromise, in the field, between good positive and negative predictive value. A PSS of 1 point identifies a low risk patient, 2 points moderate risk, 3-4 points high risk patients.
-
Early management
- Early goal directed therapy: no longer recommended. CVP is no longer required and fluid response to initial volemic reanimation has to be clinically and dynamically assessed (passive leg raise, fluid challenges)
- Fluid resuscitation: 30 ml/Kg(in the first 3 hrs) to restore normal emodynamics values (MAP >65 mmHg). Lactate is a risk assessment tool (>2 mmol/L) and is no longer recommended to guide resuscitation efforts. Crystalloids are the fluids of choice.
- Vasopressors: indicated if initial fluid resuscitation doesn’t reach the target. Norepinephrine is the pressor of choice. Epinephrine the second line agent in case Norepinephrine is not sufficiente to reach the target.Stop giving Dopamine.
- Bloodcultures: immediately and preferably before starting antibiotics but without delaying antibacterial therapy.
- Antibiotics: no double cover routinely but broad spectrum mono therapy is the recommended choice.
- Corticosteroids: consider just if patient is fully volume resuscitated and vasopressors are unsuccessful to maintain emodynamic stability.
Take home points for early phase management
Early Identification
Use either:
-
qSOFA (preferred in ED) cut off ≥2 points
-
PSS (preferred in the field) cut off ≥2 points.
Initial Management (target to a MAP >65)
-
Emodynamic stabilisation
-
1st Fluid 30 ml/Kg of crystalloids.
-
2nd Norepinephrine up to 35-90 μg/min (if 1st step failed).
-
Add Epinephrine up to 20-50 μg/min to achieve MAP target (if first 2 step failed).
-
-
Take blood cultures (if feasible before antibiotics but without delaying antibiotics).
-
Do not delay early broad spectrum antibiotic mono therapy.

References
- The Prehospital Sepsis Score. An Evidence Based Early Identification Tool.
- 2016 Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock
- The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
- A users’ guide to the 2016 Surviving Sepsis Guidelines
- 2016 NICE Sepsis: recognition, diagnosis and early management
- Raith EP, Udy AA, for the Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA. 2017;317(3):290-300. doi:10.1001/jama.2016.20328
- Freund Y, Lemachatti N, for the French Society of Emergency Medicine Collaborators Group. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA.2017;317(3):301-308. doi:10.1001/jama.2016.20329











Defibrillation Strategies: Why AHA’s position on VC and DSED is Controversial
1 FebNew 2025 Guidelines on Cardiopulmonary Resuscitation stated that alternative strategy for defibrillation of persistent VF/pVT are not yet ready for prime line based on the actual available evidences.
Previously ILCOR stated about the same topic: We suggest that a double sequential defibrillation strategy (weak recommendation, low certainty of evidence) or a vector change defibrillation strategy (weak recommendation, very low certainty of evidence) may be considered for adults with cardiac arrest who remain in ventricular fibrillation or pulseless ventricular tachycardia after 3 or more consecutive shocks.
So AHA degraded the ILCOR “may be considered to a “non useful” despite the same level of grade and evidences. Let’s see why and why THIS IS WRONG
AHA: It found significant improvement in survival at hospital discharge with VC and DSED compared to standard defibrillation by intention-to-treat, but notably not when trial findings were analyzed by the treatment strategy patients actually received
In summary, AHA highlighted one point for not suggesting VC or DSED over standard defibrillation. The reason is that the DOSE VF trial did not show any statistically relevant advantage in “per protocol analysis”!
I’m not a methodologist but I think that any of them can suffer of an heart attack hearing this statement! Intention to treat analysis is the core of randomization!
To summarize this concept here is a head to head compare between Intention to treat analysis VS per protocol analysis
In randomized control trials, analyzing patients “per protocol” removes the advantages of randomization. This choice degrades the study results to an observational level. So AHA statement is incorrect and the trial results are highly relevant
AHA: Furthermore, in a secondary exploratory analysis a significant survival benefit from DSD was only observed in the 17% of study patients in whom VF was incessant, and not in the vast majority (83%) of patients in whom VF recurred after a successful shock.
You can find the cited secondary analysis here: The impact of alternate defibrillation strategies on shock-refractory and recurrent ventricular fibrillation: A secondary analysis of the DOSE VF cluster randomized controlled trial. And the following are the results:
Shock-Refractory VF (n. 60)
Shock-Recurrent VF (n. 285)
In both cases, recurrent or persistent, even if not always statistically significant, DSD and VC performed much better than standard defibrillation WITH RESULTS ABSOLUTELY CLINICALLY RELEVANT ON ALL MAJOR OUTCOMES
AHA: The interval between each sequential “double” shock required for successfully terminating VF has also been shown experimentally (animal studies 10-100 Mses) and demonstrated in DOSE-VF itself (mean interval 650 Mses. ) to require a level of precision (separated by milliseconds) unlikely to be consistently achievable by manual activation of two defibrillators.
Th is totally wrong. The small ( 10- 100 Mses) cited from the guidelines refers to experimental animal study . DOSE-VF trial demonstrates statistically significant superiority to standard defibrillation. This superiority is observed with intervals >500 Msec that is absolutely replicable in clinical practice. The investigators also demonstrated the increase of advantages for shorter intervals. But, this increase is not seen at 10 Mses, which is only referred to in animal studies.
In case of VF/pVT. First approach:
If recurrent or refractory VF/pVT
Share this:
Tags: ACLS, ACR, arresto cardiaco, dual sequential defibrillition, emergency medicine, emergenza sanitaria territoriale, Guidelines, litterature review, medicina d'urgenza, medicina d'urgenza preospedaliera, refractory ventricular fibrillation, vector change defibrillation