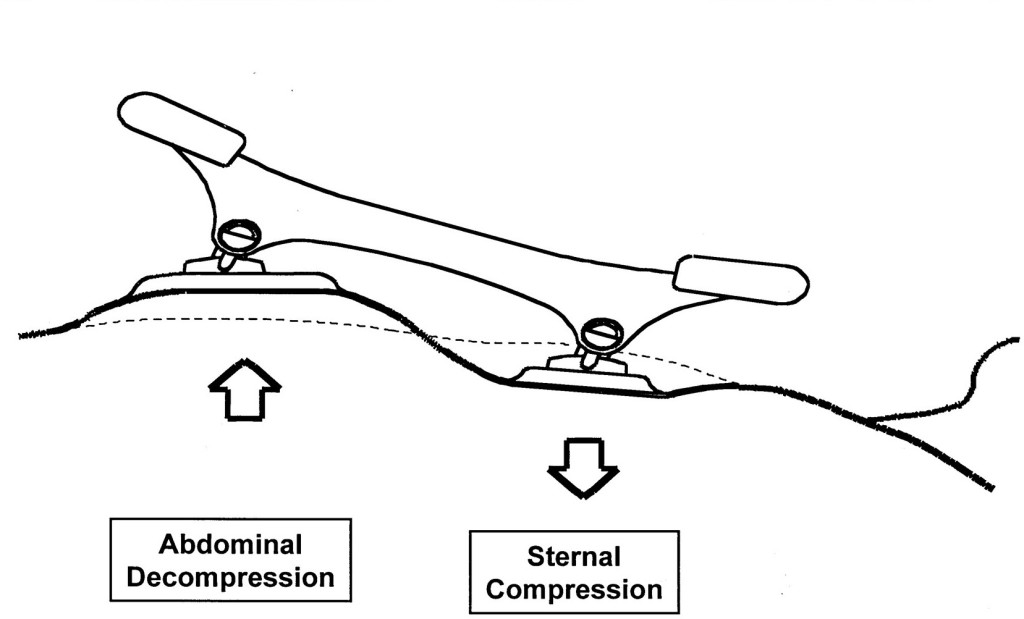
Chest compressions alternate to abdominal compression–decompression technique
Background
The abdominal compression–decompression technique is based on an “abdominal pump” model, which induces pressure changes within the abdominal cavity and promotes the return of blood from the abdominal cavity to fill the heart and be eventually pumped to the brain. A combination of abdominal compression–decompression and chest compression was previously shown to increase the venous refilling of the heart, which could generate increased coronary perfusion pressure and increase blood flow to vital organs . With this combination method, chest release during abdominal compression leads to increased venous return to the thorax by negative intrathoracic pressure. Moreover, abdominal decompression during chest compression may lead to increased blood flow via decreased afterload. In myocardial blood flow, a better 48-h outcome was documented with the combination method compared with STD-CPR
The study
This study was performed in China. It’s a single center, randomised, not blinded study.
The study aimed to compare the outcomes of standard cardiopulmonary resuscitation (STD- CPR) and combined chest compression and abdominal compression–decompression cardiopulmonary resuscitation (CO-CPR) following out-of-hospital cardiac arrest (OHCA).
Primary outcome ROSC. Secondary outcome hospital admission, hospital discharge and neurological outcome at hospital discharge.
Results
ROSC and survival to hospital admission: no statistical benefit
Survival at hospital discharge and neurological outcome: CO-CPR had statistical significant better outcome respect STD-CPR
Limitations
Single center, small sample size, no evaluation of possible abdominal injuries.
Bottom line
For prehospital use of combined chest compression and abdominal compression–decompression cardiopulmonary resuscitation we have first of all to account the need of an additional rescuer to perform abdominal compression-decompression. By the way the alternate chest/abdominal compression-decompression method is promising even if we need larger multicenter randomised trial for a more consistent evaluation of its efficacy.
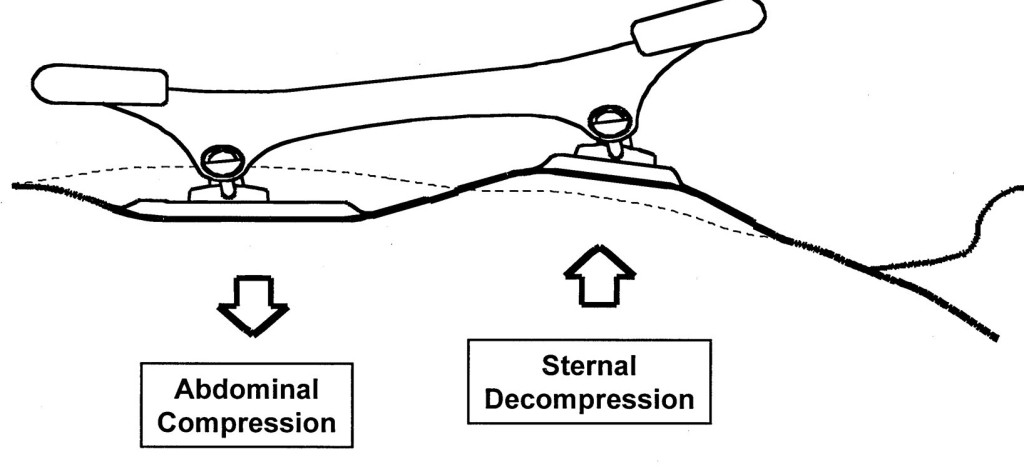
Head and thorax elevation during cardiopulmonary resuscitation

Background
Gradual elevation of the head and thorax enhances venous return from the head and neck to the thorax and further lowers intracranial pressure. This automated controlled elevation (ACE) CPR strategy consists of: (1) manual active compression decompression (ACD)-CPR and/or suction cup-based automated (LUCAS 3) CPR; (2) an impedance threshold device (ITD); and (3) an automated controlled head and thorax patient positioning device (APPD).
The study
Observational, prospective study. The Objectives of the study was to assess the probability of OHCA survival to hospital discharge after ACE-CPR versus C-CPR. ACE-CPR data were collected from a dedicated registry implemented by 10 EMS Agencies. Conventional (C) CPR data were collected from 3 large historical randomized controlled OHCA resuscitation trials.
NB: for ACE-CPR only 6/10 agencies data were evaluated.
The primary outcome was survival to hospital discharge. Secondary outcomes included ROSC at any time, and survival to hospital dis- charge with favorable neurological function.
Results
Cumulative results on primary and secondary outcome before taking into consideration the time from 911 call to ACE-CPR were not statistically significative differences. The statistical significance of ACE-CPR was reached only when time from 911 call to ACE-CPR initiation was considered.
Limitations
Observational study. Participating personnel form EMS agencies were highly motivated about ACE-CPR. 165 patients excluded with no clear explanation (generally didn’t meet inclusion criteria) from 4 EMS participating agencies. Statistical significance on primary and secondary outcome was reached after surrogate secondary analysis that considered time form 911 call to ACE-CPR start.
Bottom line
There are still insufficient historical data to understand the benefit of automated controlled elevation (ACE) CPR and this study doesn’t clear any doubt about it’s efficacies on clinical oriented outcomes.
Aortic occlusion during cardiac arrest. Mechanical adrenaline?

Background
Thoracic aortic occlusion during chest compressions limits the vascular bed for the generated cardiac output. This may increase the aortic pressure and subsequently the coronary perfusion pressure (CPP).
The coronary perfusion pressure (CPP), the pressure gradient between the aorta and right atrium, is a major determinant of the myocardial blood flow. Consequently, generating a high CPP by providing high-quality chest compression during CPR is one of the most critical factors for achieving ROSC in cardiac arrest patients.
It is uncontroversial to state that the desired effect of adrenaline in CPR is the potential increase in CPP. The potential detrimental effects of adrenaline, such as decreased cerebral blood flow, increased myocardial oxygen consumption or recurrent ventricular tachycardias after ROSC, is yet to be found with REBOA. However, adverse effects of REBOA are not reported in the limited human data published, nor has this been an endpoint in the studies conducted so far.
The study
This is a pilot study. The aim of the study was to calculate the CPP before and after REBOA balloon inflation. EtCO2 and median aortic pressure before and after balloon inflating were also measured.
Results
CPP, MAP and EtCO2 significative increased after REBOA placement in Zone 1 and balloon inflation
Limitations
Single center, small numbers, need of a large number of operators to insert the REBOA and to obtain the measurements.
Bottom line
REBOA in Cardiac Arrest is potentially useful to increase CPP and less dangerous than epinephrine administration.
It’s feasibility in emergency (in-hospital and out of hospital) settings in a timely manner and with a small number of medical personnel needs to be demonstrated.

















 of the full SOFA score outside the ICU). Non specific for sepsis.
of the full SOFA score outside the ICU). Non specific for sepsis. 







God save the King!
27 GiuMatthew E. Prekker, M.D., M.P.H., Brian E. Driver, Video versus Direct Laryngoscopy for Tracheal Intubation of Critically Ill Adults
The DirEct versus VIdeo LaryngosCopE (DEVICE) trial is a prospective, multicentre, non-blinded, randomised trial being conducted in 7 EDs and 10 ICUs in the USA
Critically ill adults undergoing tracheal intubation randomly assigned to the video-laryngoscope group or the direct-laryngoscope group
The primary outcome was successful intubation on the first attempt.
The secondary outcome was the occurrence of severe complications during intubation: severe hypoxemia, severe hypotension, new or increased vasopressor use, cardiac arrest, or death.
The trial was stopped for efficacy at the time of the single preplanned interim analysis.
Conclusions: Among critically ill adults undergoing tracheal intubation in an emergency department or ICU, the use of a videolaryngoscope resulted in a higher incidence of successful intubation on the first attempt than the use of a direct laryngoscope.
Comment: This a long journey hopefully coming to an end. From 2022 we have clear evidences on the superiority of Video versus Direct laryngoscopy Hansel J, Rogers AM, Lewis SR, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev. 2022 Apr 4;4(4):CD011136. doi: 10.1002/14651858.CD011136.pub3. PMID: 35373840; PMCID: PMC8978307.. Main airway management societies (Difficult Airway Society; Society for Airway Management; European Airway Management Society; All India Difficult Airway Society; Canadian Airway Focus Group; Safe Airway Society; and International Airway Management Society) recently updated their statements on preventing the accidental oesophageal intubation in that sense. Preventing unrecognised oesophageal intubation: a consensus guideline from the Project for Universal Management of Airways and international airway societies. The DEVICE trial is another brick in the wall of consciousness about superiority of VL vs DL despite some findings are not replicable ( ex. DL FPS 70,8%) in systems where airway management and expertise in DL is a longstanding tradition. But as said we didn’t need this trial to arrive at the conclusion of the journey.
Use the videolaryngoscope (VL) as first choice in emergent tracheal intubation to improve first passage success and prevent accidental oesophageal intubation.
Use direct laryngoscope (DL) just as rescue device in case of technical failure of the videolrayngoscope
All medical systems involved in airway management need to be aware of this. A videolaryngoscope is no longer an option but a standard equipment. The best choice is to have both, standard and hyperangulated geometry blades, in adult and paediatric sizes.
The first approach with a standard geometry blade permits to shift from VL to DL without changing device. The hyparangulated blade can be useful in selected cases even as first option..
We also consequently need to shift paradigm from classical way of teaching airway management, to a VL first approach as default method and simulating any tech failure during the practical training forcing the trainee to use the DL as rescue plan.
To let me know what is your opinion fill the survey at the link below:
VL first approach
Also read:
Condividi:
Tag:advanced airway management, Airway management, emergency medicine, litterature review, medicina d'urgenza, prehospital emergency medicine, videolaryngoscopy