Intro
The methods to confirm tracheal intubation (and exclude accidental oesophageal intubation) are classically divided in Techniques not requiring manual ventilation and Techniques requiring manual ventilation::
- Techniques not requiring manual ventilation
- Inspection of the vocal cords: there should be visual confirm- ation that the tube lies surrounded by the glottic structures
- Palpation of the trachea: an assistant palpating the external trachea may feel vibrations, corresponding to the tube passing the tracheal rings
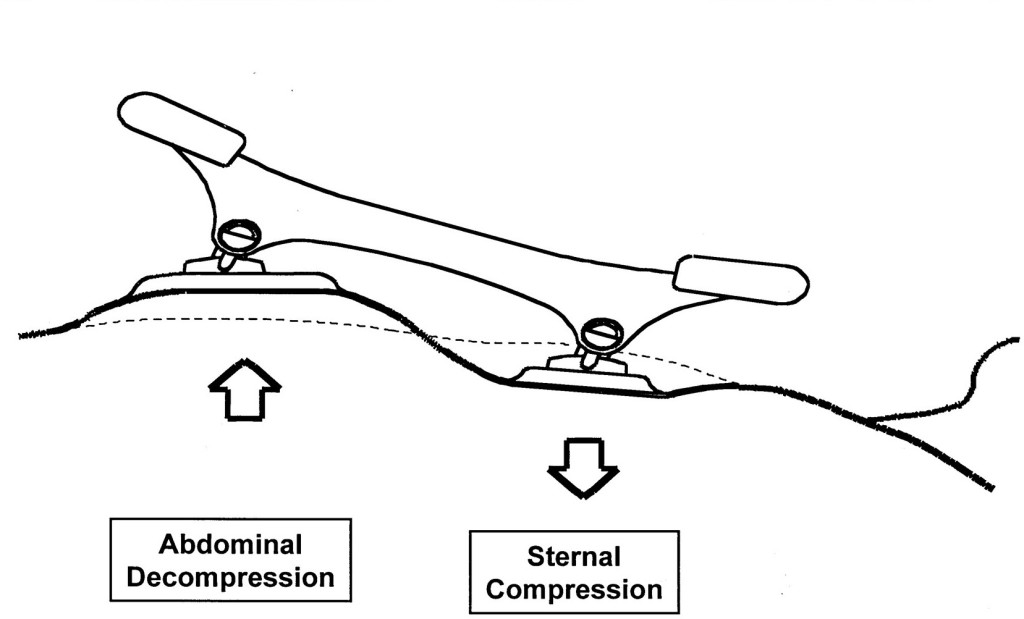
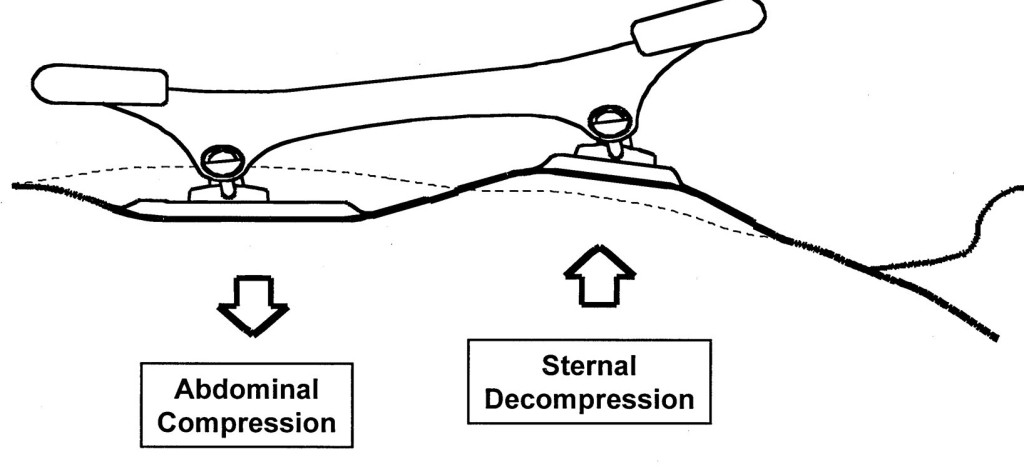
- Oesophageal detector device: Tracheal placement results in free aspiration of gas from the lungs; in oesophageal intubation, the walls of the oesophagus collapse around the tube lumen preventing gas flow
- Techniques requiring manual ventilation:
- Sounds
- Compliance: A ‘normal’ compliance during manual ventilation
- Inspection of the chest: Good expansion of the chest on manual ventilation
- Auscultation of the epigastrium
- Auscultation of the chest
- CO2 detection
- Capnography – a normal capnogram for at least six breaths suggests tracheal intubation
- Capnometry – a change in indicator to denote CO2 suggests tracheal intubation
Despite nowadays is evident that CO2 detection is the gold standard in terms of sensibility and specificity, our daily practice in managing airways still and strongly rely on clinical methods to confirm when the tube is correctly posed in the trachea and not in the oesophagus.
The article
Hansel, J., Law, J.A., Chrimes, N., Higgs, A. and Cook, T.M. (2023),
Clinical tests for confirming tracheal intubation or excluding oesophageal intubation: a diagnostic test accuracy systematic review and meta-analysis. Anaesthesia. https://doi.org/10.1111/anae.16059
In this meta-analysis the authors investigated the literature about the reliability of different methods to confirm tracheal intubation and exclude oesophageal intubation.
This is a clinically relevant point cause the unrecognised oesophageal intubation leads to catastrophic consequences on patients health.
Which Clinical test they evaluated:

How they presented the data
The false positive rate (FPR)
The FPR indicates how often any sign that is considered suggestive of successful tracheal intubation (for example chest rising or hearing breath sounds),might occur despite the tube is not in the trachea but in the oesophageal. Usually an acceptable number of FPR can be 0,1 (or the 10% (10 out of 100) of the total positive results) but you can understand how in this case, considered the high clinical relevance of the topic we have to reach for lower FPR the 1 out of 10.
The Likelihood Ratio (LR): positive (LR+) or negative (LR-)
The positive LR (LR+) indicates how many times is more probable that the tube is the trachea than in the oesophagus the investigated sign is present
A test with a LR+=10 (cut off value for reliability) means that there is 10 times more probability that the tube is really in the trachea than in the oesophagus
The negative LR (LR-) indicates how many times is more probable that the tube is the oesophagus han in the trachea if the investigated sign is present
A test with a LR- of 0.1 (cut off value for reliability) means that there is 1/10 times more probability that the tube is in the oesophagus than in the trachea.
What they found


Conclusion
The available data strongly suggest that clinical signs lack the discriminatory power to exclude oesophageal intubation to a sufficient degree to ensure patient safety when capnography is not available or doubted. The oesophageal detector device performs better than clinical examination, and in resource-limited environments with no access to capnography, may be sufficiently sensitive and specific to help guide decision-making.
Clinical Practice Take Home Message
Based on the result of this study when available use waveform capnography to confirm tracheal intubation and exclude oesophageal intubation. Clinical tests can be dangerously misleading and potentially a waste of precious time in difficult environments as emergency prehospital setting.
In poor resources systems if any form of ETCO2 is not available, the most reliable test to confirm tracheal intubation is the Oesophageal detector device.


























God save the King!
27 GiuMatthew E. Prekker, M.D., M.P.H., Brian E. Driver, Video versus Direct Laryngoscopy for Tracheal Intubation of Critically Ill Adults
The DirEct versus VIdeo LaryngosCopE (DEVICE) trial is a prospective, multicentre, non-blinded, randomised trial being conducted in 7 EDs and 10 ICUs in the USA
Critically ill adults undergoing tracheal intubation randomly assigned to the video-laryngoscope group or the direct-laryngoscope group
The primary outcome was successful intubation on the first attempt.
The secondary outcome was the occurrence of severe complications during intubation: severe hypoxemia, severe hypotension, new or increased vasopressor use, cardiac arrest, or death.
The trial was stopped for efficacy at the time of the single preplanned interim analysis.
Conclusions: Among critically ill adults undergoing tracheal intubation in an emergency department or ICU, the use of a videolaryngoscope resulted in a higher incidence of successful intubation on the first attempt than the use of a direct laryngoscope.
Comment: This a long journey hopefully coming to an end. From 2022 we have clear evidences on the superiority of Video versus Direct laryngoscopy Hansel J, Rogers AM, Lewis SR, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev. 2022 Apr 4;4(4):CD011136. doi: 10.1002/14651858.CD011136.pub3. PMID: 35373840; PMCID: PMC8978307.. Main airway management societies (Difficult Airway Society; Society for Airway Management; European Airway Management Society; All India Difficult Airway Society; Canadian Airway Focus Group; Safe Airway Society; and International Airway Management Society) recently updated their statements on preventing the accidental oesophageal intubation in that sense. Preventing unrecognised oesophageal intubation: a consensus guideline from the Project for Universal Management of Airways and international airway societies. The DEVICE trial is another brick in the wall of consciousness about superiority of VL vs DL despite some findings are not replicable ( ex. DL FPS 70,8%) in systems where airway management and expertise in DL is a longstanding tradition. But as said we didn’t need this trial to arrive at the conclusion of the journey.
Use the videolaryngoscope (VL) as first choice in emergent tracheal intubation to improve first passage success and prevent accidental oesophageal intubation.
Use direct laryngoscope (DL) just as rescue device in case of technical failure of the videolrayngoscope
All medical systems involved in airway management need to be aware of this. A videolaryngoscope is no longer an option but a standard equipment. The best choice is to have both, standard and hyperangulated geometry blades, in adult and paediatric sizes.
The first approach with a standard geometry blade permits to shift from VL to DL without changing device. The hyparangulated blade can be useful in selected cases even as first option..
We also consequently need to shift paradigm from classical way of teaching airway management, to a VL first approach as default method and simulating any tech failure during the practical training forcing the trainee to use the DL as rescue plan.
To let me know what is your opinion fill the survey at the link below:
VL first approach
Also read:
Condividi:
Tag:advanced airway management, Airway management, emergency medicine, litterature review, medicina d'urgenza, prehospital emergency medicine, videolaryngoscopy