Case presentation

You arrive on the scene of a motorbike accident. The driver, a 50 years old male, at your arrival is in “Pain” state with eyes closed and you can hear just a “snoring” sound coming from his mouth. His vitals are: NIMBP 80 over 50, HR 110, A quick primary survey reveal a low level of consciousness (eyes closed no finalised arms movement) with restored airway patency that after basic airway manoeuvres and O2 therapy (SaO2 goes to 95%) no signs of tension pneumo. A quick look to the pelvis and legs reveal a suspected “open book” lesion and a bilateral femoral fracture. No PMH is available at the moment.
Physiological response to shock
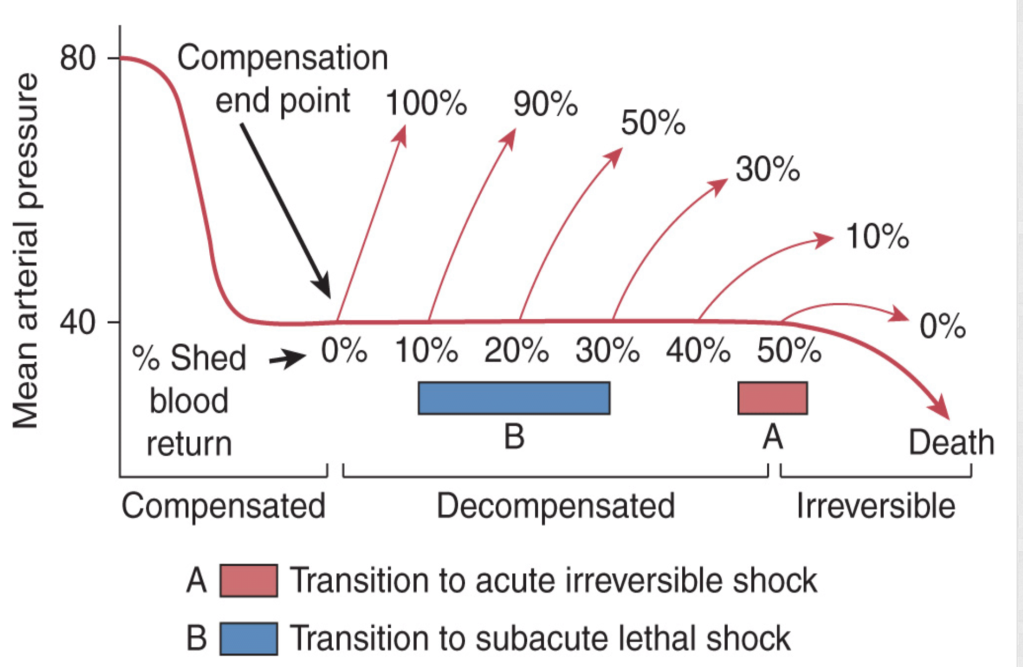
From the primary survey and vitals you can understand the patient is compensating a state of profound (hypovolemic) shock and consequent organ low perfusion with a sympathetic activation. Endogenous adrenergic mediators are trying to restore organ perfusion by vasoconstriction and increase in cardiac output.

First do not harm

Can we kill a patient destroying the physiologic response to shock?
The answer is YES! The need to protect airway performing a rapid pharmacological assisted airway management (RSI), can lead to bad consequences, destroying the physiological response to a state of profound shock.
All sedative, analgesic and anaesthetic drugs in fact antagonise and depress the sympathetic adrenergic response physiologically targeted to restore perfusion to vital organs.
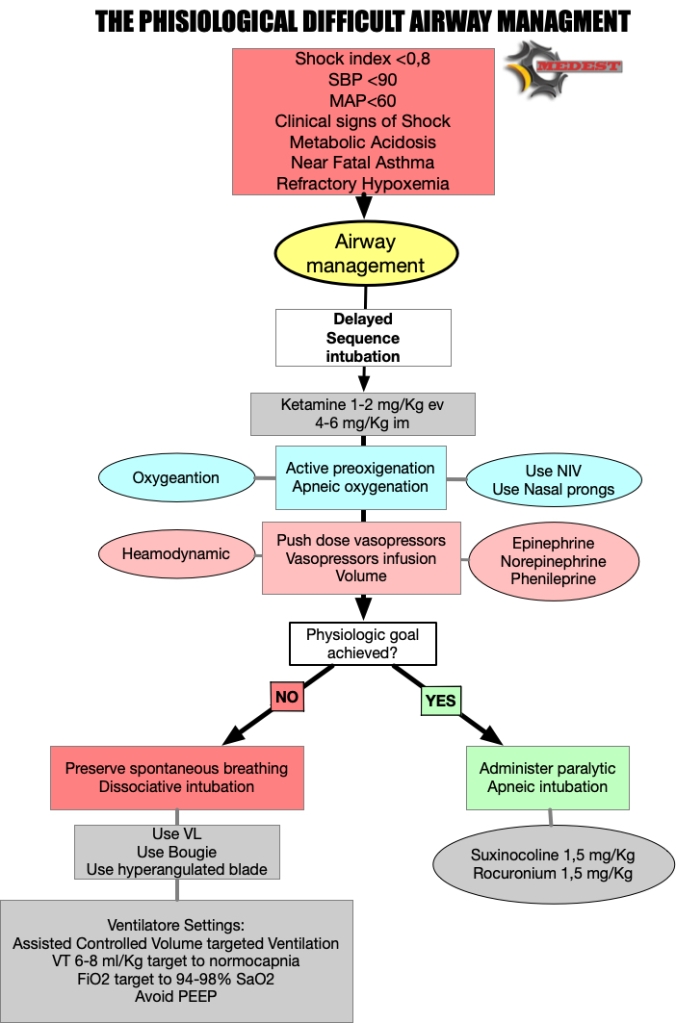
First do not harm and choose minimal emodynamic impact type and dose of drugs to perform sedation. As we know (till now) the better choice are Ketamine and Etomidate with no clear evidences on which one is preferable. We for sure know that Ketamine can be dangerous in cathecolamine depleted patients and that this effect is dose dependent. So consider using a lower dose to reach dissociative threshold being conscious that can lead to a non ideal intubation condition.
Reanimate first intubate later (aka DSI)
After a dissociative dose of Ketamine, our next clinical target is to reanimate the patient form an oxygenation and/or an organ perfusion point of view.
So we shift from a concept of Rapid Sequence Intubation to a more comprehensive plan of Delayed Sequence Airway Management. Delayed (Ketamine/Etomidate induced) to get time and reanimate, Airway Management intended as any plan (tracheal intubation, supraglottic airway) we can apply in that specific patient in the middle of the road or in other prehospital scenarios.
A properly performed pre-oxygenation with the adjunct of apneic oxygenation can restore O2 levels giving us also a good reserve for following apnea times.
Cautelative fluid administration (avoid fluids in trauma, use BLOOD) and, push dose (Epinephrine, Phenilephrine) or continuous infusion (Norepinephrine) vasopressors, can restore perfusion to abdominal and extra abdominal organs by increasing circulating volume and cardiac performance (Alfa and Beta agonist ).
Delayed paralytic administration give us the time to perform a proper reanimation reanimation and to check the effects of our interventions.
If everything goes well and the patient’s oxygenation and emodynamic state is compensated, we can administer paralytic, and go straight to perform tracheal intubation.
But if the patient remains uncompensated despite all our efforts to correct the potentially lethal cause, our last weapon can be to preserve spontaneous breathing.
Don’t live me breathless
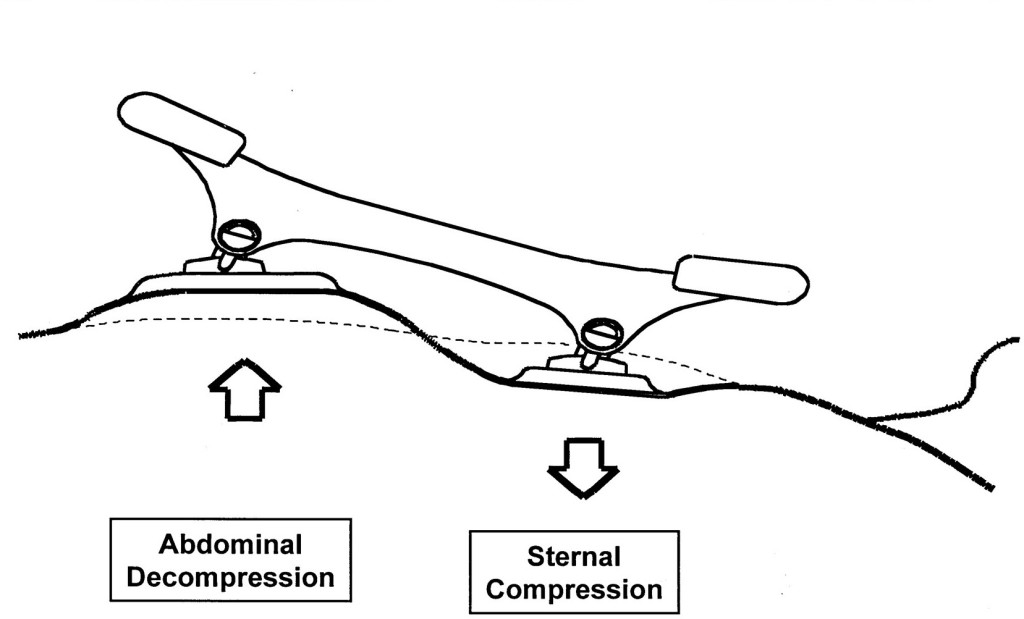
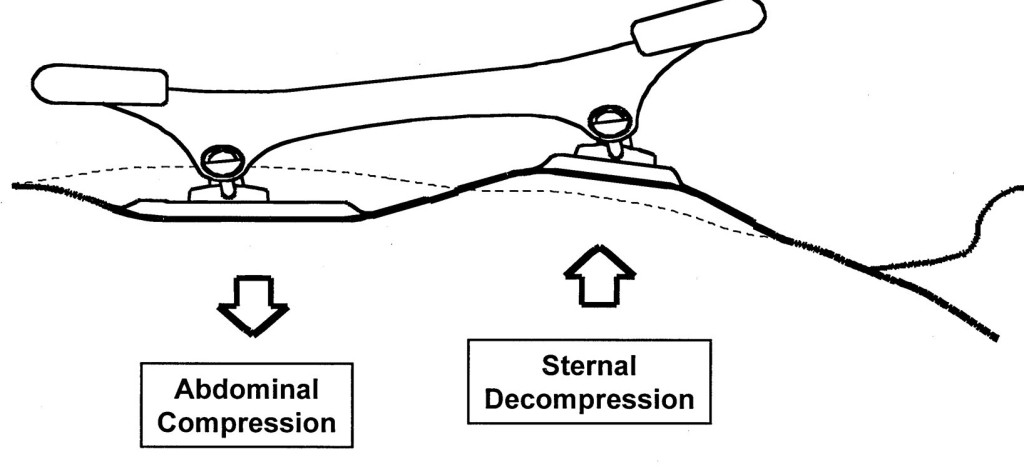
WHY? During inspiratory phase of respiratory cycle the negative intrathoracic pressure favourites venous return and increase the telediastolic volume of the left ventricle. The augmented left ventricle end diastolic pressure (LVEDP) according to Frank-Starling law improves myocardial performance increasing stroke volume and consequently cardiac output.

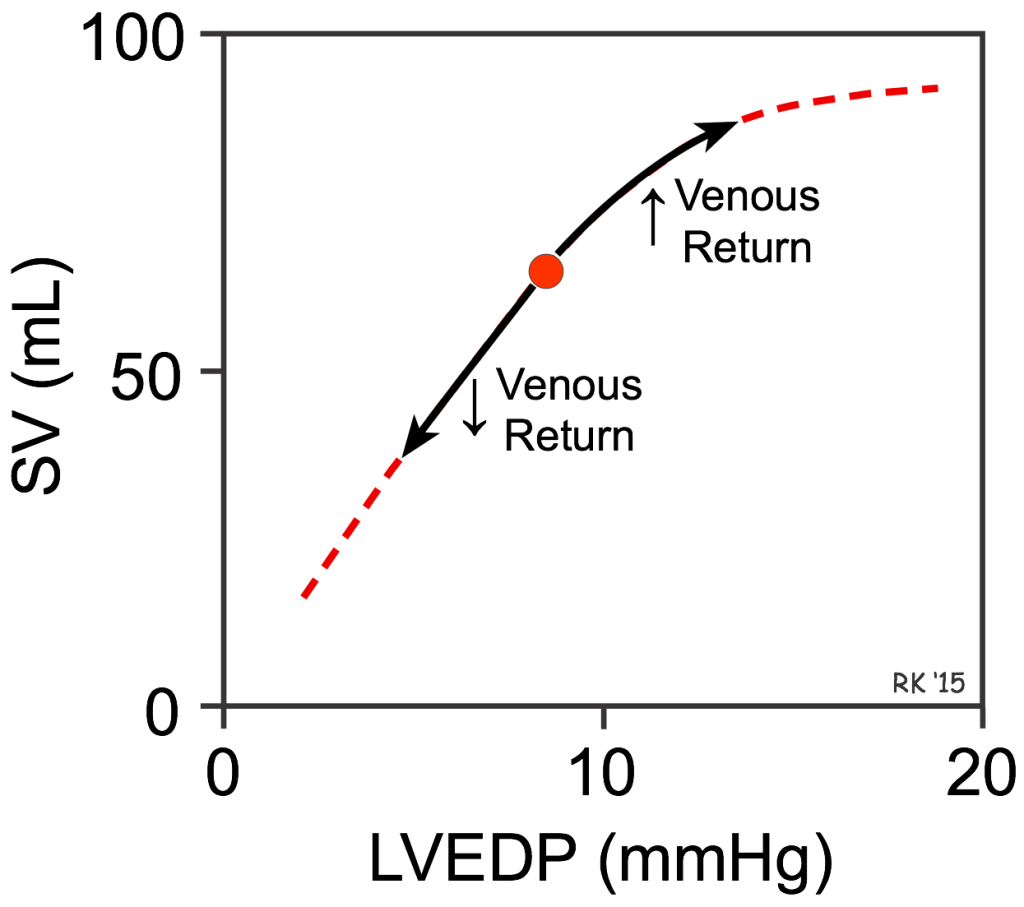
The refractory shocked patient is heavily preload dependent and suppressing the inspiratory drive risk to worsen the already dramatic emodynamic state taking him on the irreversible part of the shock curve.
We’ve got a plan
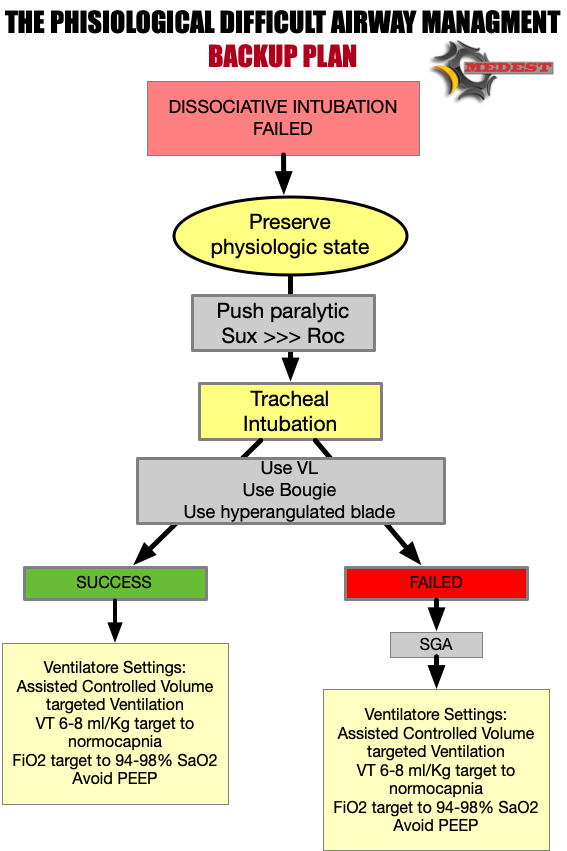
We need to have a plan for high difficult physiological airways. This is just a small residual percentage of the airways we manage in our clinical practice, but can be dramatically catastrophic when we deal with those patients without a precise plan.
We’ve got a backup plan
But when intubation fails we need to have a backup plan!
Case conclusion
You understand the need to protect patient’s airways but also the extreme physiologic difficulty of this airway.
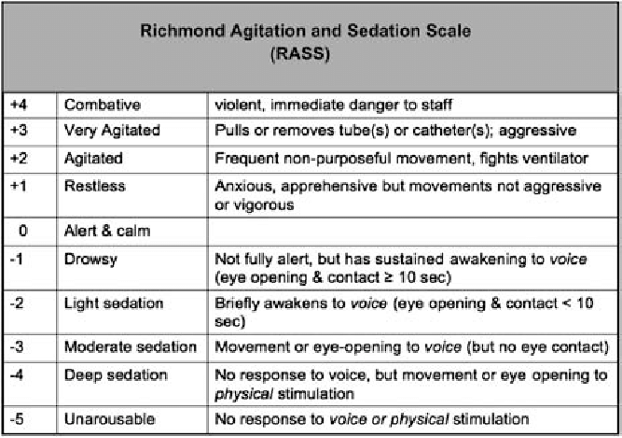
After administering a dissociative dose of Ketamine, due to the failure of any try to restore perfusion, you decide to perform a DISSOCIATIVE INTUBATION using a videolaryngoscope with a hyperangulated blade and a bougie, AVOIDING PARALYSIS.
Then you put the patient on ACV mechanical ventilation targeting a TV of 6 ml/kg and considering a “zero PEEP” strategy.
Special Thanks to Scott Weingart and Jim DuCanto for the kindness and fundamental mentorship on inspiring and peer reviewing the algorithm
References
Braude D, Palomo O, Beamsley A. Sedation only intubation. EM:RAP. 39.2013.










































God save the King!
27 GiuMatthew E. Prekker, M.D., M.P.H., Brian E. Driver, Video versus Direct Laryngoscopy for Tracheal Intubation of Critically Ill Adults
The DirEct versus VIdeo LaryngosCopE (DEVICE) trial is a prospective, multicentre, non-blinded, randomised trial being conducted in 7 EDs and 10 ICUs in the USA
Critically ill adults undergoing tracheal intubation randomly assigned to the video-laryngoscope group or the direct-laryngoscope group
The primary outcome was successful intubation on the first attempt.
The secondary outcome was the occurrence of severe complications during intubation: severe hypoxemia, severe hypotension, new or increased vasopressor use, cardiac arrest, or death.
The trial was stopped for efficacy at the time of the single preplanned interim analysis.
Conclusions: Among critically ill adults undergoing tracheal intubation in an emergency department or ICU, the use of a videolaryngoscope resulted in a higher incidence of successful intubation on the first attempt than the use of a direct laryngoscope.
Comment: This a long journey hopefully coming to an end. From 2022 we have clear evidences on the superiority of Video versus Direct laryngoscopy Hansel J, Rogers AM, Lewis SR, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev. 2022 Apr 4;4(4):CD011136. doi: 10.1002/14651858.CD011136.pub3. PMID: 35373840; PMCID: PMC8978307.. Main airway management societies (Difficult Airway Society; Society for Airway Management; European Airway Management Society; All India Difficult Airway Society; Canadian Airway Focus Group; Safe Airway Society; and International Airway Management Society) recently updated their statements on preventing the accidental oesophageal intubation in that sense. Preventing unrecognised oesophageal intubation: a consensus guideline from the Project for Universal Management of Airways and international airway societies. The DEVICE trial is another brick in the wall of consciousness about superiority of VL vs DL despite some findings are not replicable ( ex. DL FPS 70,8%) in systems where airway management and expertise in DL is a longstanding tradition. But as said we didn’t need this trial to arrive at the conclusion of the journey.
Use the videolaryngoscope (VL) as first choice in emergent tracheal intubation to improve first passage success and prevent accidental oesophageal intubation.
Use direct laryngoscope (DL) just as rescue device in case of technical failure of the videolrayngoscope
All medical systems involved in airway management need to be aware of this. A videolaryngoscope is no longer an option but a standard equipment. The best choice is to have both, standard and hyperangulated geometry blades, in adult and paediatric sizes.
The first approach with a standard geometry blade permits to shift from VL to DL without changing device. The hyparangulated blade can be useful in selected cases even as first option..
We also consequently need to shift paradigm from classical way of teaching airway management, to a VL first approach as default method and simulating any tech failure during the practical training forcing the trainee to use the DL as rescue plan.
To let me know what is your opinion fill the survey at the link below:
VL first approach
Also read:
Condividi:
Tag:advanced airway management, Airway management, emergency medicine, litterature review, medicina d'urgenza, prehospital emergency medicine, videolaryngoscopy