
Do not move! Spinal immobilization or spinal motor restriction: the long-lasting debate from the Napoleonic Wars to 2024 SIMEU policy statement

References:


Intro
The methods to confirm tracheal intubation (and exclude accidental oesophageal intubation) are classically divided in Techniques not requiring manual ventilation and Techniques requiring manual ventilation::
Despite nowadays is evident that CO2 detection is the gold standard in terms of sensibility and specificity, our daily practice in managing airways still and strongly rely on clinical methods to confirm when the tube is correctly posed in the trachea and not in the oesophagus.
The article
Hansel, J., Law, J.A., Chrimes, N., Higgs, A. and Cook, T.M. (2023),
Clinical tests for confirming tracheal intubation or excluding oesophageal intubation: a diagnostic test accuracy systematic review and meta-analysis. Anaesthesia. https://doi.org/10.1111/anae.16059
In this meta-analysis the authors investigated the literature about the reliability of different methods to confirm tracheal intubation and exclude oesophageal intubation.
This is a clinically relevant point cause the unrecognised oesophageal intubation leads to catastrophic consequences on patients health.
Which Clinical test they evaluated:

How they presented the data
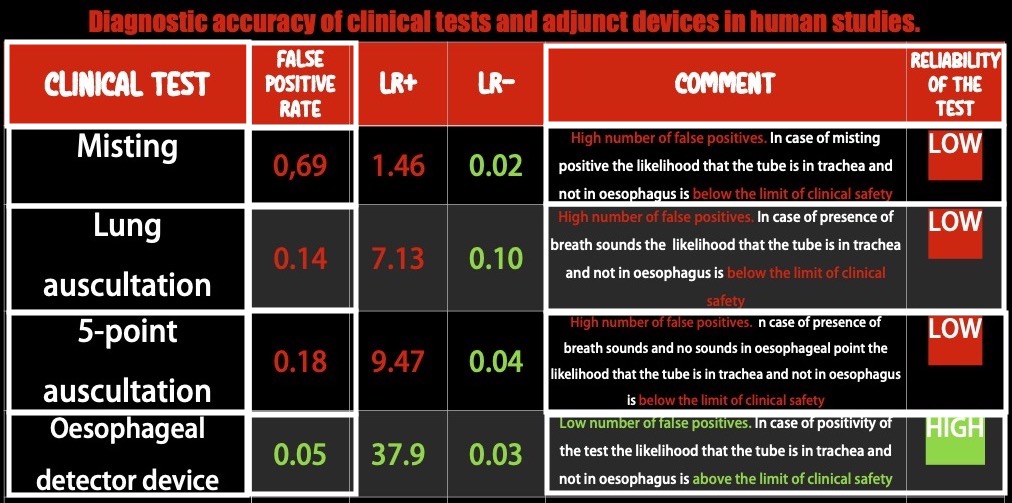
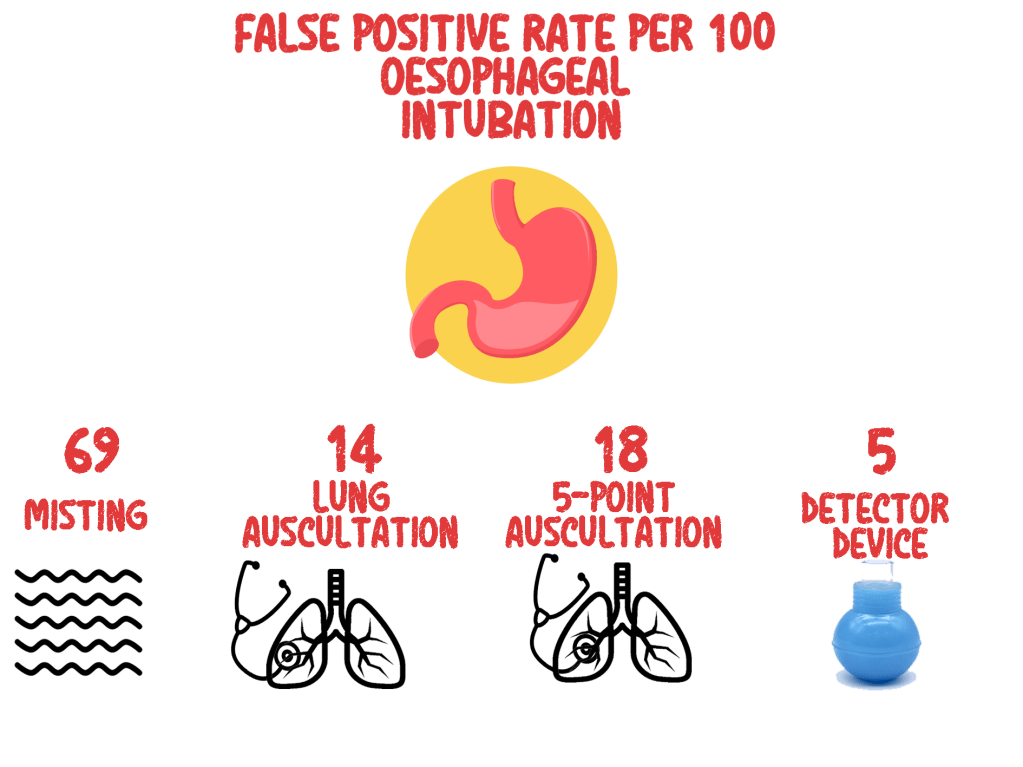
The FPR indicates how often any sign that is considered suggestive of successful tracheal intubation (for example chest rising or hearing breath sounds),might occur despite the tube is not in the trachea but in the oesophageal. Usually an acceptable number of FPR can be 0,1 (or the 10% (10 out of 100) of the total positive results) but you can understand how in this case, considered the high clinical relevance of the topic we have to reach for lower FPR the 1 out of 10.
The positive LR (LR+) indicates how many times is more probable that the tube is the trachea than in the oesophagus the investigated sign is present
A test with a LR+=10 (cut off value for reliability) means that there is 10 times more probability that the tube is really in the trachea than in the oesophagus
The negative LR (LR-) indicates how many times is more probable that the tube is the oesophagus han in the trachea if the investigated sign is present
A test with a LR- of 0.1 (cut off value for reliability) means that there is 1/10 times more probability that the tube is in the oesophagus than in the trachea.
What they found
Conclusion
The available data strongly suggest that clinical signs lack the discriminatory power to exclude oesophageal intubation to a sufficient degree to ensure patient safety when capnography is not available or doubted. The oesophageal detector device performs better than clinical examination, and in resource-limited environments with no access to capnography, may be sufficiently sensitive and specific to help guide decision-making.
Clinical Practice Take Home Message
Based on the result of this study when available use waveform capnography to confirm tracheal intubation and exclude oesophageal intubation. Clinical tests can be dangerously misleading and potentially a waste of precious time in difficult environments as emergency prehospital setting.
In poor resources systems if any form of ETCO2 is not available, the most reliable test to confirm tracheal intubation is the Oesophageal detector device.


The DirEct versus VIdeo LaryngosCopE (DEVICE) trial is a prospective, multicentre, non-blinded, randomised trial being conducted in 7 EDs and 10 ICUs in the USA
Critically ill adults undergoing tracheal intubation randomly assigned to the video-laryngoscope group or the direct-laryngoscope group
The primary outcome was successful intubation on the first attempt.
The secondary outcome was the occurrence of severe complications during intubation: severe hypoxemia, severe hypotension, new or increased vasopressor use, cardiac arrest, or death.
The trial was stopped for efficacy at the time of the single preplanned interim analysis.

Comment: This a long journey hopefully coming to an end. From 2022 we have clear evidences on the superiority of Video versus Direct laryngoscopy Hansel J, Rogers AM, Lewis SR, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev. 2022 Apr 4;4(4):CD011136. doi: 10.1002/14651858.CD011136.pub3. PMID: 35373840; PMCID: PMC8978307.. Main airway management societies (Difficult Airway Society; Society for Airway Management; European Airway Management Society; All India Difficult Airway Society; Canadian Airway Focus Group; Safe Airway Society; and International Airway Management Society) recently updated their statements on preventing the accidental oesophageal intubation in that sense. Preventing unrecognised oesophageal intubation: a consensus guideline from the Project for Universal Management of Airways and international airway societies. The DEVICE trial is another brick in the wall of consciousness about superiority of VL vs DL despite some findings are not replicable ( ex. DL FPS 70,8%) in systems where airway management and expertise in DL is a longstanding tradition. But as said we didn’t need this trial to arrive at the conclusion of the journey.
All medical systems involved in airway management need to be aware of this. A videolaryngoscope is no longer an option but a standard equipment. The best choice is to have both, standard and hyperangulated geometry blades, in adult and paediatric sizes.
The first approach with a standard geometry blade permits to shift from VL to DL without changing device. The hyparangulated blade can be useful in selected cases even as first option..
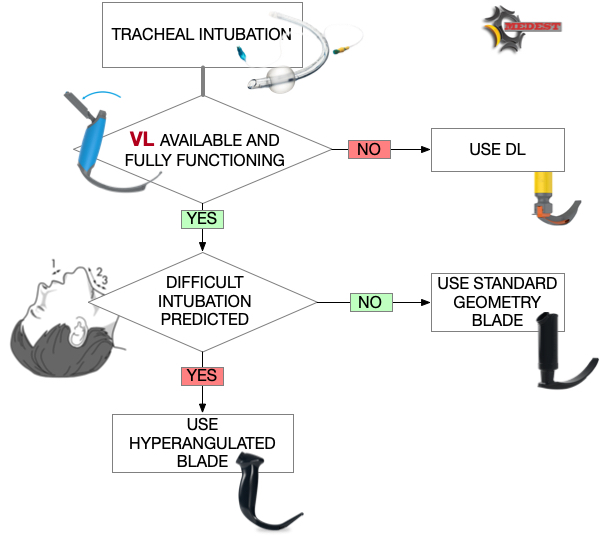
We also consequently need to shift paradigm from classical way of teaching airway management, to a VL first approach as default method and simulating any tech failure during the practical training forcing the trainee to use the DL as rescue plan.
To let me know what is your opinion fill the survey at the link below:
Also read:



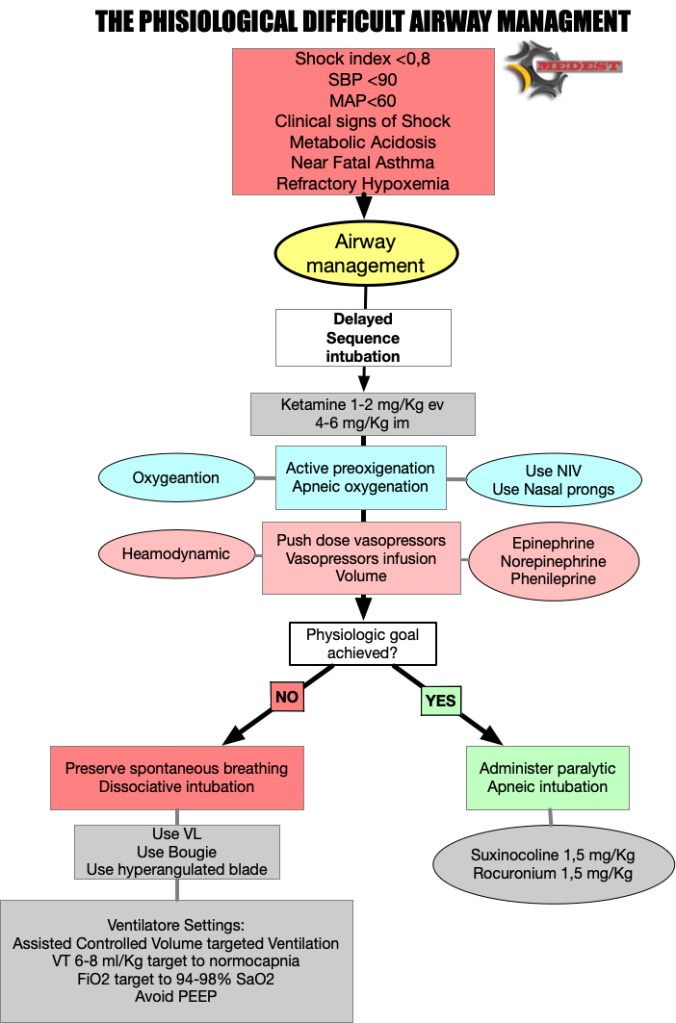
You arrive on the scene of a motorbike accident. The driver, a 50 years old male, at your arrival is in “Pain” state with eyes closed and you can hear just a “snoring” sound coming from his mouth. His vitals are: NIMBP 80 over 50, HR 110, A quick primary survey reveal a low level of consciousness (eyes closed no finalised arms movement) with restored airway patency that after basic airway manoeuvres and O2 therapy (SaO2 goes to 95%) no signs of tension pneumo. A quick look to the pelvis and legs reveal a suspected “open book” lesion and a bilateral femoral fracture. No PMH is available at the moment.
From the primary survey and vitals you can understand the patient is compensating a state of profound (hypovolemic) shock and consequent organ low perfusion with a sympathetic activation. Endogenous adrenergic mediators are trying to restore organ perfusion by vasoconstriction and increase in cardiac output.

Can we kill a patient destroying the physiologic response to shock?
The answer is YES! The need to protect airway performing a rapid pharmacological assisted airway management (RSI), can lead to bad consequences, destroying the physiological response to a state of profound shock.
All sedative, analgesic and anaesthetic drugs in fact antagonise and depress the sympathetic adrenergic response physiologically targeted to restore perfusion to vital organs.
First do not harm and choose minimal emodynamic impact type and dose of drugs to perform sedation. As we know (till now) the better choice are Ketamine and Etomidate with no clear evidences on which one is preferable. We for sure know that Ketamine can be dangerous in cathecolamine depleted patients and that this effect is dose dependent. So consider using a lower dose to reach dissociative threshold being conscious that can lead to a non ideal intubation condition.
After a dissociative dose of Ketamine, our next clinical target is to reanimate the patient form an oxygenation and/or an organ perfusion point of view.
So we shift from a concept of Rapid Sequence Intubation to a more comprehensive plan of Delayed Sequence Airway Management. Delayed (Ketamine/Etomidate induced) to get time and reanimate, Airway Management intended as any plan (tracheal intubation, supraglottic airway) we can apply in that specific patient in the middle of the road or in other prehospital scenarios.
A properly performed pre-oxygenation with the adjunct of apneic oxygenation can restore O2 levels giving us also a good reserve for following apnea times.
Cautelative fluid administration (avoid fluids in trauma, use BLOOD) and, push dose (Epinephrine, Phenilephrine) or continuous infusion (Norepinephrine) vasopressors, can restore perfusion to abdominal and extra abdominal organs by increasing circulating volume and cardiac performance (Alfa and Beta agonist ).
Delayed paralytic administration give us the time to perform a proper reanimation reanimation and to check the effects of our interventions.
If everything goes well and the patient’s oxygenation and emodynamic state is compensated, we can administer paralytic, and go straight to perform tracheal intubation.
But if the patient remains uncompensated despite all our efforts to correct the potentially lethal cause, our last weapon can be to preserve spontaneous breathing.
WHY? During inspiratory phase of respiratory cycle the negative intrathoracic pressure favourites venous return and increase the telediastolic volume of the left ventricle. The augmented left ventricle end diastolic pressure (LVEDP) according to Frank-Starling law improves myocardial performance increasing stroke volume and consequently cardiac output.

The refractory shocked patient is heavily preload dependent and suppressing the inspiratory drive risk to worsen the already dramatic emodynamic state taking him on the irreversible part of the shock curve.

We need to have a plan for high difficult physiological airways. This is just a small residual percentage of the airways we manage in our clinical practice, but can be dramatically catastrophic when we deal with those patients without a precise plan.
But when intubation fails we need to have a backup plan!
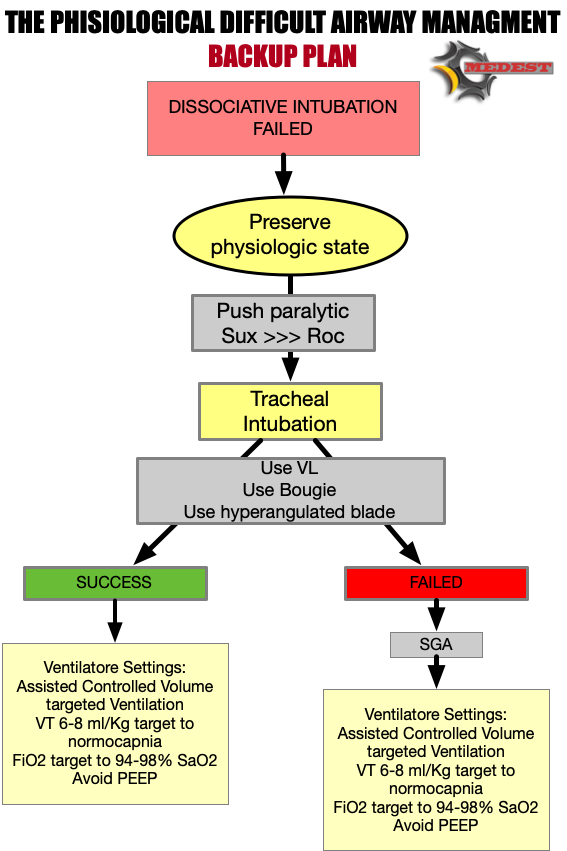
You understand the need to protect patient’s airways but also the extreme physiologic difficulty of this airway.
After administering a dissociative dose of Ketamine, due to the failure of any try to restore perfusion, you decide to perform a DISSOCIATIVE INTUBATION using a videolaryngoscope with a hyperangulated blade and a bougie, AVOIDING PARALYSIS.
Then you put the patient on ACV mechanical ventilation targeting a TV of 6 ml/kg and considering a “zero PEEP” strategy.
Special Thanks to Scott Weingart and Jim DuCanto for the kindness and fundamental mentorship on inspiring and peer reviewing the algorithm
Braude D, Palomo O, Beamsley A. Sedation only intubation. EM:RAP. 39.2013.



The abdominal compression–decompression technique is based on an “abdominal pump” model, which induces pressure changes within the abdominal cavity and promotes the return of blood from the abdominal cavity to fill the heart and be eventually pumped to the brain. A combination of abdominal compression–decompression and chest compression was previously shown to increase the venous refilling of the heart, which could generate increased coronary perfusion pressure and increase blood flow to vital organs . With this combination method, chest release during abdominal compression leads to increased venous return to the thorax by negative intrathoracic pressure. Moreover, abdominal decompression during chest compression may lead to increased blood flow via decreased afterload. In myocardial blood flow, a better 48-h outcome was documented with the combination method compared with STD-CPR
This study was performed in China. It’s a single center, randomised, not blinded study.
The study aimed to compare the outcomes of standard cardiopulmonary resuscitation (STD- CPR) and combined chest compression and abdominal compression–decompression cardiopulmonary resuscitation (CO-CPR) following out-of-hospital cardiac arrest (OHCA).
Primary outcome ROSC. Secondary outcome hospital admission, hospital discharge and neurological outcome at hospital discharge.
ROSC and survival to hospital admission: no statistical benefit
Survival at hospital discharge and neurological outcome: CO-CPR had statistical significant better outcome respect STD-CPR
Single center, small sample size, no evaluation of possible abdominal injuries.
For prehospital use of combined chest compression and abdominal compression–decompression cardiopulmonary resuscitation we have first of all to account the need of an additional rescuer to perform abdominal compression-decompression. By the way the alternate chest/abdominal compression-decompression method is promising even if we need larger multicenter randomised trial for a more consistent evaluation of its efficacy.

Gradual elevation of the head and thorax enhances venous return from the head and neck to the thorax and further lowers intracranial pressure. This automated controlled elevation (ACE) CPR strategy consists of: (1) manual active compression decompression (ACD)-CPR and/or suction cup-based automated (LUCAS 3) CPR; (2) an impedance threshold device (ITD); and (3) an automated controlled head and thorax patient positioning device (APPD).
Observational, prospective study. The Objectives of the study was to assess the probability of OHCA survival to hospital discharge after ACE-CPR versus C-CPR. ACE-CPR data were collected from a dedicated registry implemented by 10 EMS Agencies. Conventional (C) CPR data were collected from 3 large historical randomized controlled OHCA resuscitation trials.
NB: for ACE-CPR only 6/10 agencies data were evaluated.
The primary outcome was survival to hospital discharge. Secondary outcomes included ROSC at any time, and survival to hospital dis- charge with favorable neurological function.
Cumulative results on primary and secondary outcome before taking into consideration the time from 911 call to ACE-CPR were not statistically significative differences. The statistical significance of ACE-CPR was reached only when time from 911 call to ACE-CPR initiation was considered.
Observational study. Participating personnel form EMS agencies were highly motivated about ACE-CPR. 165 patients excluded with no clear explanation (generally didn’t meet inclusion criteria) from 4 EMS participating agencies. Statistical significance on primary and secondary outcome was reached after surrogate secondary analysis that considered time form 911 call to ACE-CPR start.
There are still insufficient historical data to understand the benefit of automated controlled elevation (ACE) CPR and this study doesn’t clear any doubt about it’s efficacies on clinical oriented outcomes.

Thoracic aortic occlusion during chest compressions limits the vascular bed for the generated cardiac output. This may increase the aortic pressure and subsequently the coronary perfusion pressure (CPP).
The coronary perfusion pressure (CPP), the pressure gradient between the aorta and right atrium, is a major determinant of the myocardial blood flow. Consequently, generating a high CPP by providing high-quality chest compression during CPR is one of the most critical factors for achieving ROSC in cardiac arrest patients.
It is uncontroversial to state that the desired effect of adrenaline in CPR is the potential increase in CPP. The potential detrimental effects of adrenaline, such as decreased cerebral blood flow, increased myocardial oxygen consumption or recurrent ventricular tachycardias after ROSC, is yet to be found with REBOA. However, adverse effects of REBOA are not reported in the limited human data published, nor has this been an endpoint in the studies conducted so far.
This is a pilot study. The aim of the study was to calculate the CPP before and after REBOA balloon inflation. EtCO2 and median aortic pressure before and after balloon inflating were also measured.
CPP, MAP and EtCO2 significative increased after REBOA placement in Zone 1 and balloon inflation
Single center, small numbers, need of a large number of operators to insert the REBOA and to obtain the measurements.
REBOA in Cardiac Arrest is potentially useful to increase CPP and less dangerous than epinephrine administration.
It’s feasibility in emergency (in-hospital and out of hospital) settings in a timely manner and with a small number of medical personnel needs to be demonstrated.


Just published Preventing unrecognised oesophageal intubation: a consensus guideline from the Project for Universal Management of Airways and international airway societies
Thanks to a prestigious panel of international authors. Great job and definitely solid indication about how to prevent and recognise accidental oesophageal intubation.
Just some of the key recommendations
Refer to the full text guidelines for more.
Here is the link to Safe Airway Society livestream event.
Must read, must follow. Free open access.

The following are personal considerations on peculiar aspects about management of accidental oesophageal intubation in prehospital environment and come from my personal clinical experience.
Beware they are just personal considerations and practical tricks and tips and are not intended to substitute the above guidelines.
They are intended to suggest an alternative mental and technical approach when dealing with oesophageal intubation on uncontrolled patients in difficult environment.

DO NOT REMOVE THE OT TUBE STRAIGHT FORWARD IN CASE OF ACCIDENTAL OESOPHAGEAL INTUBATION IN PREHOSPITAL ENVIRONMENT.



Supporting ALL Ohio EM Residencies in the #FOAMed World
Let's try to make it simple
a blog for thinking docs: blending good evidence, physiology, common sense, and applying it at the bedside!
More definitive diagnosis, better patient care
Reviewing Critical Care, Journals and FOAMed
Prehospital critical care for out-of-hospital cardiac arrest
Education and entertainment for the ultrasound enthusiast
A UK PREHOSPITAL PODCAST
Emergency medicine - When minutes matter...
Sharing the Science and Art of Paediatric Anaesthesia
"Live as if you will die tomorrow; Learn as if you will live forever"
Navigating resuscitation
A Hive Mind for Prehospital and Retrieval Med
Thoughts and opinions on airways and resuscitation science
A Free Open Access Medical Education Emergency Medicine Core Content Mash Up
Rural Generalist Doctors Education
Emergency Medicine #FOAMed
این سایت را به آن دکتوران و محصلین طب که شب و روز برای رفاه نوع انسان فداکاری می کنند ، جوانی و لذایذ زندگی را بدون چشمداشت به امتیاز و نفرین و آفرین قربان خدمت به بشر می کنند و بار سنگین خدمت و اصلاح را بدوش می کشند ، اهداء می کنم This site is dedicated to all Doctors and students that aver the great responsibility of People’s well-being upon their shoulders and carry on their onerous task with utmost dedication and Devotionاولین سایت و ژورنال انتــرنتی علـــمی ،تخـصصی ، پــژوهشــی و آمــوزشــی طبـــی در افغــانســـتان
PHARM, #FOAMed
Free Open Access Medical Education
Learning everything I can from everywhere I can. This is my little blog to keep track of new things medical, paramedical and pre-hospital from a student's perspective.
In memory of Dr John Hinds
All you want to know about prehospital emergency medicine
Check out our updated blog posts at https://www.italycustomized.it/blog
The FOAM Search Engine
where everything is up for debate . . .
Pediatric Emergency Medicine Education
Free Open Access Medical Education for Paramedics
useful resources for rural clinicians
Unofficial site for prehospital care providers of the Auckland HEMS service
L'ECOGRAFIA: ENTROPIA DELL'IMMAGINE
Prehospital Emergency Medicine
Your Boot Camp Guide to Emergency Medicine
WE HAVE MOVED - VISIT WWW.KIDOCS.ORG FOR NEW CONTENT
Prehospital Emergency Medicine
Academic Medicine Pearls in Emergency Medicine from THE Ohio State University Residency Program
Prehospital Emergency Medicine
Prehospital Emergency Medicine
The Pre-Hospital & Retrieval Medicine Team of NSW Ambulance
Safer Ventilation Strategies
28 LugCondividi: