Main changes in recommendations
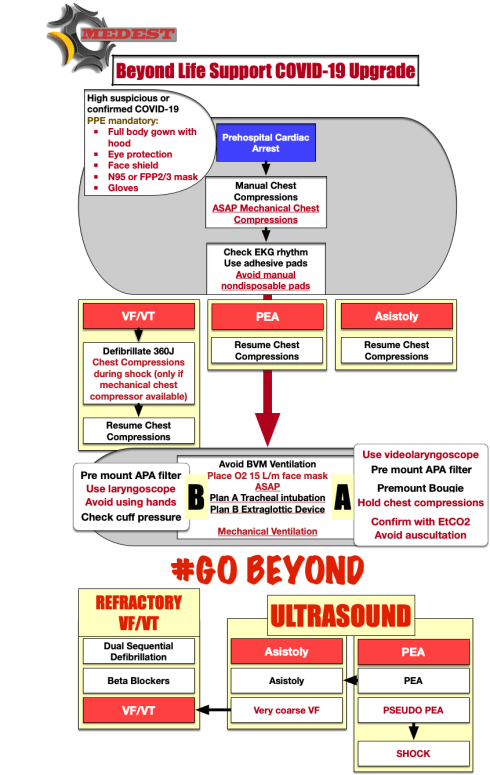
Personal Protective Equipment for Advanced Life Support interventions need to be at maximum level of protection of full body, eyes and airways.
CAT 3 level of protection 4 (at least) for the full body
FPP2/N95 airway filter for team members who are NOT directly involved in airway management, ventilation or manual chest compressions
FPP3/N99 airway filter for providers who are directly involved in airway management, ventilation and manual chest compressions.
Face shield and protective googles are strongly suggested
Mechanical Chest compressors devices are the gold standard to perform cardiac massage. They reduce contacts and contamination risk and team member exposure to contaminants.
Adhesive disposable pads are the only option to check rhythm and deliver shock. Dispose non-disposable, manual pads.
Passive O2 administration (via simple face mack at a rate of 15l/m) during chest compressions is the first option over bag mask ventilation when performing Basic Life Support waiting for advanced airway management.When using a Bag Valve Mask always put a HEPA/HME filter between Bag and mask to avoid contamination
Hold chest compressions when performing airway managment
Cover patient head with a transparent plastic foil to minimise virus spreading and contamination when performing airway management and bag mask ventilation
Tracheal intubation using a video laryngoscope is the first line option for advanced airway management to minimise contamination.
If video laryngoscope is not available Extraglottic devices are an acceptable first line option
Use all the implementation to improve intubation first passage success:
Video laringoscopy
Bougie
RAMP positioning
Suctioning (SALAD technique)
Use all the implementation to improve Extraglottic device placement
Laryngoscope for tongue displacement and mouth opening (DO NOT USE hands)
Deflate cuff
Lubrificate the device
Whatever plan you apply use an HEPA/HME filter immediately after the ventilation device
Use disposable cover and disposable gel to perform Ultrasound during chest compressions
- References
- AHA. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19
- European Resuscitation Council COVID-19 Guidelines
- Italian Resuscitation Council. Raccomandazioni per la Rianimazione Cardiopolmonare (RCP) durante l’epidemia da Sars-Cov-2 e in caso di sospetta o confermata infezione Covid-19







Defibrillation Strategies: Why AHA’s position on VC and DSED is Controversial
1 FebNew 2025 Guidelines on Cardiopulmonary Resuscitation stated that alternative strategy for defibrillation of persistent VF/pVT are not yet ready for prime line based on the actual available evidences.
Previously ILCOR stated about the same topic: We suggest that a double sequential defibrillation strategy (weak recommendation, low certainty of evidence) or a vector change defibrillation strategy (weak recommendation, very low certainty of evidence) may be considered for adults with cardiac arrest who remain in ventricular fibrillation or pulseless ventricular tachycardia after 3 or more consecutive shocks.
So AHA degraded the ILCOR “may be considered to a “non useful” despite the same level of grade and evidences. Let’s see why and why THIS IS WRONG
AHA: It found significant improvement in survival at hospital discharge with VC and DSED compared to standard defibrillation by intention-to-treat, but notably not when trial findings were analyzed by the treatment strategy patients actually received
In summary, AHA highlighted one point for not suggesting VC or DSED over standard defibrillation. The reason is that the DOSE VF trial did not show any statistically relevant advantage in “per protocol analysis”!
I’m not a methodologist but I think that any of them can suffer of an heart attack hearing this statement! Intention to treat analysis is the core of randomization!
To summarize this concept here is a head to head compare between Intention to treat analysis VS per protocol analysis
In randomized control trials, analyzing patients “per protocol” removes the advantages of randomization. This choice degrades the study results to an observational level. So AHA statement is incorrect and the trial results are highly relevant
AHA: Furthermore, in a secondary exploratory analysis a significant survival benefit from DSD was only observed in the 17% of study patients in whom VF was incessant, and not in the vast majority (83%) of patients in whom VF recurred after a successful shock.
You can find the cited secondary analysis here: The impact of alternate defibrillation strategies on shock-refractory and recurrent ventricular fibrillation: A secondary analysis of the DOSE VF cluster randomized controlled trial. And the following are the results:
Shock-Refractory VF (n. 60)
Shock-Recurrent VF (n. 285)
In both cases, recurrent or persistent, even if not always statistically significant, DSD and VC performed much better than standard defibrillation WITH RESULTS ABSOLUTELY CLINICALLY RELEVANT ON ALL MAJOR OUTCOMES
AHA: The interval between each sequential “double” shock required for successfully terminating VF has also been shown experimentally (animal studies 10-100 Mses) and demonstrated in DOSE-VF itself (mean interval 650 Mses. ) to require a level of precision (separated by milliseconds) unlikely to be consistently achievable by manual activation of two defibrillators.
Th is totally wrong. The small ( 10- 100 Mses) cited from the guidelines refers to experimental animal study . DOSE-VF trial demonstrates statistically significant superiority to standard defibrillation. This superiority is observed with intervals >500 Msec that is absolutely replicable in clinical practice. The investigators also demonstrated the increase of advantages for shorter intervals. But, this increase is not seen at 10 Mses, which is only referred to in animal studies.
In case of VF/pVT. First approach:
If recurrent or refractory VF/pVT
Share this:
Tags: ACLS, ACR, arresto cardiaco, dual sequential defibrillition, emergency medicine, emergenza sanitaria territoriale, Guidelines, litterature review, medicina d'urgenza, medicina d'urgenza preospedaliera, refractory ventricular fibrillation, vector change defibrillation