Intro
The methods to confirm tracheal intubation (and exclude accidental oesophageal intubation) are classically divided in Techniques not requiring manual ventilation and Techniques requiring manual ventilation::
- Techniques not requiring manual ventilation
- Inspection of the vocal cords: there should be visual confirm- ation that the tube lies surrounded by the glottic structures
- Palpation of the trachea: an assistant palpating the external trachea may feel vibrations, corresponding to the tube passing the tracheal rings
- Oesophageal detector device: Tracheal placement results in free aspiration of gas from the lungs; in oesophageal intubation, the walls of the oesophagus collapse around the tube lumen preventing gas flow
- Techniques requiring manual ventilation:
- Sounds
- Compliance: A ‘normal’ compliance during manual ventilation
- Inspection of the chest: Good expansion of the chest on manual ventilation
- Auscultation of the epigastrium
- Auscultation of the chest
- CO2 detection
- Capnography – a normal capnogram for at least six breaths suggests tracheal intubation
- Capnometry – a change in indicator to denote CO2 suggests tracheal intubation
Despite nowadays is evident that CO2 detection is the gold standard in terms of sensibility and specificity, our daily practice in managing airways still and strongly rely on clinical methods to confirm when the tube is correctly posed in the trachea and not in the oesophagus.
The article
Hansel, J., Law, J.A., Chrimes, N., Higgs, A. and Cook, T.M. (2023),
Clinical tests for confirming tracheal intubation or excluding oesophageal intubation: a diagnostic test accuracy systematic review and meta-analysis. Anaesthesia. https://doi.org/10.1111/anae.16059
In this meta-analysis the authors investigated the literature about the reliability of different methods to confirm tracheal intubation and exclude oesophageal intubation.
This is a clinically relevant point cause the unrecognised oesophageal intubation leads to catastrophic consequences on patients health.
Which Clinical test they evaluated:

How they presented the data
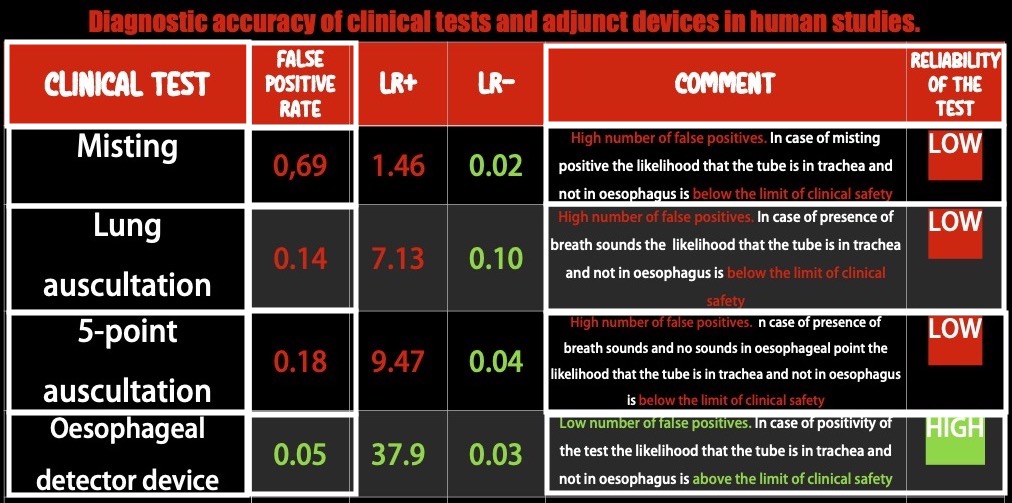
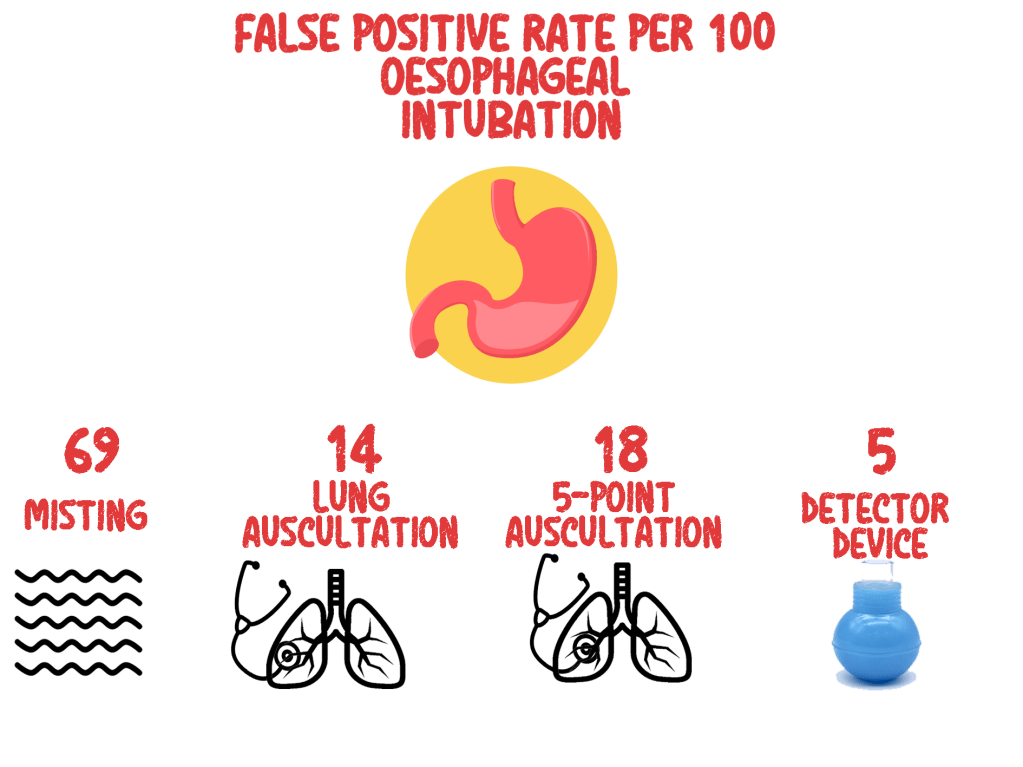
The false positive rate (FPR)
The FPR indicates how often any sign that is considered suggestive of successful tracheal intubation (for example chest rising or hearing breath sounds),might occur despite the tube is not in the trachea but in the oesophageal. Usually an acceptable number of FPR can be 0,1 (or the 10% (10 out of 100) of the total positive results) but you can understand how in this case, considered the high clinical relevance of the topic we have to reach for lower FPR the 1 out of 10.
The Likelihood Ratio (LR): positive (LR+) or negative (LR-)
The positive LR (LR+) indicates how many times is more probable that the tube is the trachea than in the oesophagus the investigated sign is present
A test with a LR+=10 (cut off value for reliability) means that there is 10 times more probability that the tube is really in the trachea than in the oesophagus
The negative LR (LR-) indicates how many times is more probable that the tube is the oesophagus han in the trachea if the investigated sign is present
A test with a LR- of 0.1 (cut off value for reliability) means that there is 1/10 times more probability that the tube is in the oesophagus than in the trachea.
What they found
Conclusion
The available data strongly suggest that clinical signs lack the discriminatory power to exclude oesophageal intubation to a sufficient degree to ensure patient safety when capnography is not available or doubted. The oesophageal detector device performs better than clinical examination, and in resource-limited environments with no access to capnography, may be sufficiently sensitive and specific to help guide decision-making.
Clinical Practice Take Home Message
Based on the result of this study when available use waveform capnography to confirm tracheal intubation and exclude oesophageal intubation. Clinical tests can be dangerously misleading and potentially a waste of precious time in difficult environments as emergency prehospital setting.
In poor resources systems if any form of ETCO2 is not available, the most reliable test to confirm tracheal intubation is the Oesophageal detector device.



In case of oesophageal intubation
19 AugJust published Preventing unrecognised oesophageal intubation: a consensus guideline from the Project for Universal Management of Airways and international airway societies
Thanks to a prestigious panel of international authors. Great job and definitely solid indication about how to prevent and recognise accidental oesophageal intubation.
Just some of the key recommendations
Refer to the full text guidelines for more.
Here is the link to Safe Airway Society livestream event.
Must read, must follow. Free open access.
Let’s go outside
The following are personal considerations on peculiar aspects about management of accidental oesophageal intubation in prehospital environment and come from my personal clinical experience.
Beware they are just personal considerations and practical tricks and tips and are not intended to substitute the above guidelines.
They are intended to suggest an alternative mental and technical approach when dealing with oesophageal intubation on uncontrolled patients in difficult environment.
Some general considerations
DO NOT REMOVE THE OT TUBE STRAIGHT FORWARD IN CASE OF ACCIDENTAL OESOPHAGEAL INTUBATION IN PREHOSPITAL ENVIRONMENT.
The way I like it. The way I do it.
Suitability
Feasibility
The visual algorithm
The Video
Share this: