General considerations (dyspneic non infective patients)
Self Protection
The generic dyspneic patients do not pose any particular self protection issues above the general precautions
Clinical needs
Non infected dyspneic patient need moderately high FiO2 but considerately high oxygen flow rates.
The available systems we have in this moment (at least on my operative setting) to deliver normally pressured O2 are:
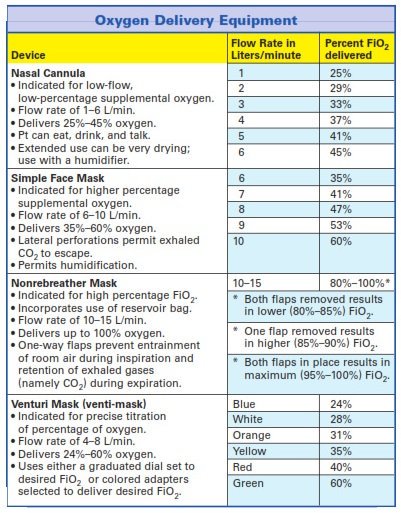
- Nasal cannula
- Maximum gas flow 15 l/m
- FiO2 variable between 25-45%
- Simple face mask
- Maximum gas flow 15 l/m
- FiO2 variable between 40-60% at the mask level
- Nonrebreather face mask (reservoir)
- Maximum gas flow 15 l/m
- FiO2 more 80-100%
- Venturi mask
- Gas flow between 40 to over 80 l/m
- FiO2 titratable between 24% and 60%
To satisfy the increased minute ventilation of the highly dyspneic patient Venturi mask is the best device (high flow rate) and permits at the same time to tritrate the FiO2 based on the patients need avoiding indiscriminate hyperoxygenation.
Particular considerations in dyspneic potentially infective COVID-19 patients
Disclaimer
The following considerations derived from our initial experience on the field in suspect or confirmed COVID-19 with respiratory symptoms at their presentation or in the initial phases. Those are the majority of the patients we observed till the day this post was written.
The following considerations are not intended for all the severe hypoxic patients who definitively need early intubation and positive pressure ventilation.
Clinical needs
Those are dyspneic hypoxic patients who needs moderately high FiO2 and request more gas flow rates to satisfy increased minute ventilation.
So from an exclusively clinical point of view the best way to deliver oxygen it would be a Venturi mask.
Self Protection
In the actual situation in Italy the epidemiological geographical criteria is no more reliable to identify COVID-19 patients so any prehospital healthcare professional providing direct care to a dyspneic patient needs to be protected al least with:
-
- Eye protection or Facial shield
- Medical mask
- Disposable gown
- Disposable gloves
At the same time good practice is to reduce at minimum the number of direct caring providers, to maintain, if possible, a security distance > 1 mt, to invite any patient to wear, if tolerated, a surgical mask, and a pair of disposable gloves to minimise the risk of infection.
When providing direct care of dyspneic patients who needs O2 therapy the level of risk for droplet diffusion is generally increased cause of the presence of the gas flow.
All the available systems for oxygen delivery we mentioned above are open and allow a free exaltation of the patient in the surrounding area and potentially exposes all the healthcare caregivers to an increased risk of contamination cause of the augmented droplet dispersion and to a lack of protection.
Considerations
So when dealing with O2 therapy in the potentially infected patients we need to consider the relationship between risk of contamination and clinical efficacy of any device.
Nasal Cannula
-
Oxygenation –—+
-
Protection ++++
Nasal Cannula is the only device that permits the patient to wear a surgical mask on nose and mouth, decreasing droplet diffusion and protecting the healthcare team and at the same time maintains a certain clinical efficacy..
So my first approach is Nasal Cannula underneath a medical mask.
Utilising a different device than nasal cannula plus medical mask on the patient mouth and nose (simple, non rebreather or Venturi face mask) to deliver oxygen therapy all healthcare professionals need to be aware that the risk infection increases and the patient has no barriers and so they have to consider improving his own self protection level (N95, FPP2 mask at least)
Simple/Non rebreather Facial Mask
-
Oxygenation —++
-
Protection ++–
When you can’t reach a clinical acceptable SpO2 with nasal cannula we need to downgrade on our first goal (protection) to achieve a better clinical outcome.
Simple facial masks maintain a moderate protection form droplet spreading with a more clinical efficacy respect th the nasal cannula.
Nonrebreather facial mask either moderately protects against droplet diffusion with an improvement in FiO2 above simple face mask but the nonrebreather bag is a potential expirate gas reservoir potentially increasing the risk of spreading.
Venturi mask
-
Oxygenation -++++
-
Protection —-+
High flow titratable FiO2 in an open system mask can satisfy all minute ventilation needing guaranteeing Oxygenation at a cost of a great risk of spreading. My last choice in the scale of conventional Oxygen therapy.
References:
DSC Hui, MTV Chan, B Chow. Aerosol dispersion during various respiratory therapies: a risk assessment model of nosocomial infection to health care workers. Hong Kong Med J 2014;20(Suppl 4):S9-13
M. P. Wan , C. Y. H. Chao , Y. D. Ng , G. N. Sze To & W. C. Yu (2007) Dispersion of Expiratory Droplets in a General Hospital Ward with Ceiling Mixing Type Mechanical Ventilation System, Aerosol Science and Technology, 41:3, 244-258, DOI: 10.1080/02786820601146985
Shu-An Lee, Dong-Chir Hwang, He-Yi Li, Chieh-Fu Tsai, Chun-Wan Chen,and Jen-Kun Chen. Particle Size-Selective Assessment of Protection of
European Standard FFP Respirators and Surgical Masks against Particles-Tested with Human Subjects. Journal of Healthcare Engineering. Volume 2016, Article ID 8572493, 12 pages
Thanks for reviewing and suggesting to: Scott Weingart, Jim DuCanto, Velia Marta Antonini, Giacomo Magagnotti, Andrea Paoli and all the other colleagues and friends who supported this post










Respiratory support in suspected COVID-19 patients. When conventional O2 therapy is not enough!
20 MarWe talk about evidences on respiratory support in the dyspneic and moderately/severe hypoxic suspect COVID-19 patient on the field. Clinical evidences and contamination risks in the potentially infected COV 19 patients to guide our efforts toward a good outcome when the conventional O2 therapy is not enough.
A step backward
The COVID-19 pneumonia. More than a “baby lung”
Clinical features and Imaging in early phases
Lung mechanics
Evidences of clinical features of OneLevel (CPAP) and BiLevel (BiPAP) respiratory support in massive epidemic crisis.
Not much of that. NIV in SARS and MERS epidemic demonstrated a poor outcome over invasive mechanical ventilation and possible delay effect on tracheal intubation and mechanical ventilation.
Clinical features OneLevel respiratory support
Clinical features BiLevel respiratory support
Risk benefits assessment
More risk patient level
More risk device level
Droplet spreading. OneLevel VS BiLevel respiratory support
Prehospital strategy and practical tips
When high flow conventional O2 therapy is not enough to reach clinical goals in the highly risk patient, non otherwise transportable and at risk of rapidly loosing airway patency One level PEEP respiratory support (CPAP) is the best compromise between clinical efficacy and contamination risk.
Ventilatory inspiratory support (BiPAP) doesn’t add much from a clinical point of view and increase the risk of contamination so has to be avoided.
Practical tips when using CPAP on the field
References
Share this: