From a practical clinical point of view, after the 2016 update of the SSC (Surviving Sepsis Campaign) guidelines we have two references when comes to deal with a potential septic patient. 
2016 Sepsis 3 definition and early management.
2016 Surviving Sepsis Campaign
Let’s see how to treat, based on top evidences, a real patient in the the pre-hospital and emergency department time window.
But, first of all, the definitions:
Both the guidelines now agree that:
“Sepsis should be defined as life-threatening organ dysfunction caused by a dysregulated host response to infection“
“Septic shock should be defined as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by a vasopressor requirement to maintain a mean arterial pressure of 65 mm Hg or greater and serum lactate level greater than 2 mmol/L (>18 mg/dL) despite adequate volume resuscitation”
-
Early identification
- SIRS criteria. The new 2016 SSC guidelines do not indicate any criteria for early identification of sepsis, so SIRS criteria no longer exists.
- qSOFA score (G.C.S. of 13 or less, SBP of 100 mm Hg or less, and RR 22/min or greater): Good negative and positive prediction value(similar to that
 of the full SOFA score outside the ICU). Non specific for sepsis. It’s the actual early identification tool for sepsis to use out-of-hospital end in emergency department. It performs quite good to identify patients at risk of negative evolution. A qSOFA score ≥2 indicates a high mortality risk comparing to a qSOFA ≤1.
of the full SOFA score outside the ICU). Non specific for sepsis. It’s the actual early identification tool for sepsis to use out-of-hospital end in emergency department. It performs quite good to identify patients at risk of negative evolution. A qSOFA score ≥2 indicates a high mortality risk comparing to a qSOFA ≤1.

- SOFA score: indicates organ disfunction (when the score is >2 points) consequent to the infection and defines sepsis. Is a validated ICU tool to asses risk and mortality chance. Is not a tool to use out-of-hospital or in ED.
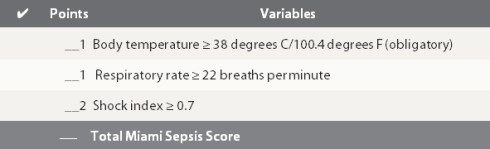
- The Pre-hospital Sepsis Score (PSS) or Miami Sepsis Score: As out-of-hospital professional I love pre-hospital early warning tools.I like to mention PSS cause is well validated to early recognise sepsis in the field. PSS includes Shock Index (HR/SBP) that is really sensible to identify critical evolution chance, RR that is included in qSOFA and other sepsis score plus body temperature (obligatory) that identifies an infection. Is for me the good compromise, in the field, between good positive and negative predictive value. A PSS of 1 point identifies a low risk patient, 2 points moderate risk, 3-4 points high risk patients.
-
Early management
- Early goal directed therapy: no longer recommended. CVP is no longer required and fluid response to initial volemic reanimation has to be clinically and dynamically assessed (passive leg raise, fluid challenges)
- Fluid resuscitation: 30 ml/Kg(in the first 3 hrs) to restore normal emodynamics values (MAP >65 mmHg). Lactate is a risk assessment tool (>2 mmol/L) and is no longer recommended to guide resuscitation efforts. Crystalloids are the fluids of choice.
- Vasopressors: indicated if initial fluid resuscitation doesn’t reach the target. Norepinephrine is the pressor of choice. Epinephrine the second line agent in case Norepinephrine is not sufficiente to reach the target.Stop giving Dopamine.
- Bloodcultures: immediately and preferably before starting antibiotics but without delaying antibacterial therapy.
- Antibiotics: no double cover routinely but broad spectrum mono therapy is the recommended choice.
- Corticosteroids: consider just if patient is fully volume resuscitated and vasopressors are unsuccessful to maintain emodynamic stability.
Take home points for early phase management
Early Identification
Use either:
-
qSOFA (preferred in ED) cut off ≥2 points
-
PSS (preferred in the field) cut off ≥2 points.
Initial Management (target to a MAP >65)
-
Emodynamic stabilisation
-
1st Fluid 30 ml/Kg of crystalloids.
-
2nd Norepinephrine up to 35-90 μg/min (if 1st step failed).
-
Add Epinephrine up to 20-50 μg/min to achieve MAP target (if first 2 step failed).
-
Take blood cultures (if feasible before antibiotics but without delaying antibiotics).
-
Do not delay early broad spectrum antibiotic mono therapy.

References
Tags: Guidelines, Sepsis, Sepsis 3, Surviving Sepsis Campaign
Le tue opinioni sono il nostro valore aggiunto!

Sepsis: Sepsis 3, Surviving Sepsis Campaign what now?
23 JanFrom a practical clinical point of view, after the 2016 update of the SSC (Surviving Sepsis Campaign) guidelines we have two references when comes to deal with a potential septic patient.
2016 Sepsis 3 definition and early management.
2016 Surviving Sepsis Campaign
Let’s see how to treat, based on top evidences, a real patient in the the pre-hospital and emergency department time window.
But, first of all, the definitions:
Definitions
Both the guidelines now agree that:
“Sepsis should be defined as life-threatening organ dysfunction caused by a dysregulated host response to infection“
“Septic shock should be defined as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by a vasopressor requirement to maintain a mean arterial pressure of 65 mm Hg or greater and serum lactate level greater than 2 mmol/L (>18 mg/dL) despite adequate volume resuscitation”
Early identification
Early management
Take home points for early phase management
Early Identification
Use either:
qSOFA (preferred in ED) cut off ≥2 points
PSS (preferred in the field) cut off ≥2 points.
Initial Management (target to a MAP >65)
Emodynamic stabilisation
1st Fluid 30 ml/Kg of crystalloids.
2nd Norepinephrine up to 35-90 μg/min (if 1st step failed).
Add Epinephrine up to 20-50 μg/min to achieve MAP target (if first 2 step failed).
Take blood cultures (if feasible before antibiotics but without delaying antibiotics).
Do not delay early broad spectrum antibiotic mono therapy.
References
Share this:
Tags: Guidelines, Sepsis, Sepsis 3, Surviving Sepsis Campaign